Policies and Procedures: Difference between revisions
| Line 3,695: | Line 3,695: | ||
::1. The NIH utilizes a zoned evacuation system. When and if the fire alarm signal sounds and the flashing emergency strobe light has been activated in a particular area the occupants in that zone or area of the building must evacuate the building. This alarm is usually followed by recorded instructions to the occupants. Other areas may not be required to evacuate unless their zone fire alarm system has been activated as well. |
::1. The NIH utilizes a zoned evacuation system. When and if the fire alarm signal sounds and the flashing emergency strobe light has been activated in a particular area the occupants in that zone or area of the building must evacuate the building. This alarm is usually followed by recorded instructions to the occupants. Other areas may not be required to evacuate unless their zone fire alarm system has been activated as well. |
||
| ⚫ | |||
<br> |
|||
| ⚫ | |||
:: |
::3. During a fire emergency: |
||
::::a. The ETL will be responsible for the orderly evacuation of and accounting for all staff, subjects and visitors; |
::::a. The ETL will be responsible for the orderly evacuation of and accounting for all staff, subjects and visitors; |
||
::::b. The ATL will help to carry out the instructions of the ETL and assists all patients / visitors in the case of an evacuation. |
::::b. The ATL will help to carry out the instructions of the ETL and assists all patients / visitors in the case of an evacuation. |
||
| Line 3,716: | Line 3,715: | ||
|} |
|} |
||
:: |
::4. If there is a small fire which may be contained using a fire extinguisher: |
||
::::a. The nearest fire extinguisher is located outside the MEG Lab. |
::::a. The nearest fire extinguisher is located outside the MEG Lab. |
||
::::b. Extinguish the fire only if it can be done without endangering anyone, after notifying the NIH Fire Department. |
::::b. Extinguish the fire only if it can be done without endangering anyone, after notifying the NIH Fire Department. |
||
| Line 3,735: | Line 3,734: | ||
|} |
|} |
||
::5. '''Fire Evacuation Procedures:''' |
|||
::::a. Close all doors as you leave (close the MSR door if safe to do so). |
::::a. Close all doors as you leave (close the MSR door if safe to do so). |
||
::::b. Walk to the nearest FIRE ALARM PULL STATION which is located in the NMR Center main corridor on the wall between the Waiting Area and the door leading to the main building; activate the alarm. |
::::b. Walk to the nearest FIRE ALARM PULL STATION which is located in the NMR Center main corridor on the wall between the Waiting Area and the door leading to the main building; activate the alarm. |
||
Revision as of 12:04, 18 August 2018
Policies and Procedures Manual
These documents comprise the official policies and procedures for the MEG lab.
Operations
Hours of Operation
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
- 1) Normal hours of operations 9:00-5:00 pm Monday - Friday. The MEG Core Facility staff will be available to assist users during normal hours of operation. The MEG Core Facility staff MAY be able to assist users outside these hours, at their discretion, with prior authorization and notice of at least one week; please see the MEG Core staff Request Form (under construction).
- 2) Users may schedule scans for after hours provided they are certified as an authorized independent user, and conduct studies in accordance with MEG policies and procedures. Please see User Guidelines for further information.
Laboratory Access
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
- 1) MEG Users will be given the MEG Lab keyless entry code during the MEG Orientation Training class.
- 2) During Normal Hours of Operations- the MEG Lab may or may not be locked, however, if locked access may be gained / the door can be unlocked by using the access code.
- 3) After Normal Hours of Operations and on the weekends- the MEG Lab will be locked, however, access can be gained by using the keyless entry system.
- 4) All equipment, except for all computers (acquisition and workstation) and electronics, must be powered off upon departure.
- 5) It will be the responsibility of the user to make sure the lab is locked upon departure.
- 6) After hours access to the NMR Center, which houses the MEG Lab, is given at the discretion of the NMR Center staff.
User and Safety Guidelines
Policy governing user requirements and laboratory safety
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- I. Becoming a User: Training and Authorization
- 1. MEG Orientation
- a. Users must schedule / attend an official MEG orientation to become familiar with the lab operations and equipment. Any personnel present in the MEG laboratory during acquisition must complete the MEG orientation, including all clinical support staff.
- 1. MEG Orientation
- 2. Authorized Independent User Requirements
- At least one of the persons in attendance at every MEG session must be authorized to operate the MEG independently. The authorization process involves several steps. To become authorized, the user is expected to become competent in performing all aspects of MEGs. MEG Core staff is available to provide training and technical assistance. Steps to becoming an authorized independent user appear below.
- a. The first step in becoming an authorized independent user is to attend the MEG Orientation.
- b. Following completion of the orientation, each new user must assist with a minimum of two (2) MEG sessions, and independently perform one additional MEG session, in the presence of MEG Core facility staff or an authorized trainer. Additional observed sessions may be required to achieve competency. To request MEG Core Staff assistance/training use the MEG Core Staff Request Form (Under construction).
- c. Scientific staff in NIMH IRP labs at the doctoral level with at least one full year of experience as an independent user may be named as an authorized trainer at the discretion of the MEG core facility.
- d. Post-baccalaureate IRTA trainees can become authorized independent users, although they may not serve as authorized trainers.
- e. New users who have performed all procedures in the presence of MEG Core staff (or an authorized trainer) and have attained competency in all skills will be added to the authorized independent user list. The authorized independent user list and the authorized trainer list will be maintained by the lab manager and technologist, Judy Mitchell.
- II. Initiating a MEG Study
- 1. Study Design Review and Approval
- II. Initiating a MEG Study
- a. Users must provide the director and/or staff scientist with a description of the research study design including information regarding setup requirements, software, and equipment needs.
- 1. Protocol Approval
- a. User groups are required to have an IRB approved protocol with a description of the intended MEG research before any human subjects can be scanned.
- 1. Protocol Approval
- b. Established users with new protocols will be required to complete a “new” Facility Access Request for each new protocol indicating the new protocol number; see Facility Access Requests and Scheduling below.
- 4. Routine Studies
- a. The MEG core facility requires that at least two persons are present in the room at every MEG session. Both persons must have completed the MEG orientation. One person must be monitoring the subject inside the MSR at all times. One person may be clinical support staff. One person may be MEG Core facility staff, with prior approval and notice of at least one week. Please use the MEG Core Staff Request Form (Under construction)
- b. One of the two persons present at every MEG session must be authorized to operate the MEG independently (or must be MEG core facility staff). The next session details the authorization procedure.
- c. Any invasive studies (i.e. studies involving infusions, blood draws, etc.) must be accompanied by personnel with NIH CC clinical credentials. This person must have completed the MEG orientation, and can also serve as the second person.
- d. Upon review of the IRB approved protocol for non-invasive studies involving research subjects who are not classified as healthy volunteers, the MEG core facility may require NIH CC credentialed staff to be present during recordings.
- e. One person must be monitoring the subject in the MSR at all times.
- 2. Equipment Testing / Task Setup
- a. The MEG Core facility recommends initial pilot testing of task paradigm, equipment, software, etc. without a research subject.
- b. MEG Core staff are available, upon request, to assist in troubleshooting during pilot testing, with at least one week's notice. Please indicate the need for any special training, i.e., training or assistance with EEG/EP electrode placement or setup on the MEG Core Staff Request Form (Under construction)
- c. Users must schedule time via the web calendar for all testing. When scheduling indicate in the scheduling module that the appointment is for "pilot testing: no subject".
- 3. Pilot Studies
- a. The MEG Core facility recommends a pilot study to test equipment, paradigms / programs and refine procedures with a test subject. Users must provide their own volunteer subject; if this is an external volunteer, he/she must be consented according to IRB guidelines.
- b. MEG Core staff are available, upon request, to assist during pilot testing, with at least one week's notice. Please indicate the need for any special support. Please use the MEG Core Staff Request Form (Under construction).
- c. You must schedule time for the pilot study via the web calendar. Please indicate in the description that time is being requested for a “pilot study”.
- d. Pilot studies with a subject are required to have two persons in attendance who have completed the MEG orientation (in addition to the subject). One person may be MEG Core facility staff.
- III. User Log
- Users MUST document any scan that they perform in the User Log Book. If a subject was set up for the MEG but the scan was not performed – that scan must still be logged in the User Log Book with a comment explaining why the study was not performed.
- Subject information and all other pertinent information must be filled out in the log book, i.e., date, PI name, operator’s initials, protocol #, subject’s initials, MRN, and the gantry position. Do not leave any blank entries.
- IV. Lab Safety
- 1. Equipment Operation - When performing a MEG study there must be at least two persons assisting with a study; one person must be an authorized independent user and both persons must have completed the MEG orientation.
- IV. Lab Safety
- 2. Subject Safety – a subject must never be left alone in the MSR without an investigator in the control room for any reason. The subject must be observed by an investigator at all times. Violation of this procedure may lead to revocation of lab access priveleges.
- 3. Chair / Table Safety – Care should be taken when raising the chair / table when you have a subject sitting or supine in the gantry. Operating instructions are below in Chair Operation. The chair has a 300 lbs. maximum weight limit, and the bed (for supine recording) has a weight limit of 250 lbs.
- 4. Gantry Safety – Never adjust the gantry (tilt or angle) when a subject is seated in the chair or lying on the table. Instructions are available in Gantry Operation.
- 5. If a medical emergency occurs call 111. For Fire or Police call 911. For any other emergency contact the director or staff scientist for assistance at the phone numbers posted in the lab.
- V. User Feedback and Problem Reporting
- 1. User Feedback – Users are encouraged to make suggestions and provide feedback to MEG staff, by directly contacting the staff scientist (Tom Holroyd) and director (Allison Nugent).
- 2. Problem Reporting – Users are responsible for reporting complications, incidents, or problems that occur involving the facility via the Problem Report Form (under construction). Any variance/problem occurring that affected subject safety should be reported immediately to the institute clinical director and the IRB by the investigators in addition the the MEG Core director; reporting of unanticipated problems or adverse events to the IRB is not the responsibility of the MEG Core facility.
- 3. Equipment Failure -Users are also responsible for reporting any equipment failure or any equipment that may not be working properly via the Problem Report Form (under construction). Any equipment that is inoperable or broken should be labeled as such, and the staff scientist (Tom Holroyd), Director (Allison Nugent) and Lab Technologist (Judy Mitchell) should be informed immediately.
- V. User Feedback and Problem Reporting
- VI. Magnetically Shielded Room (MSR) Guidelines
- There are no known risks associated with MEG/EEG recordings. Although wearing metal objects while in the MSR (Magnetically Shielded Room) is not harmful to the individual, bringing metal objects in the MSR can result in a poor quality / uninterruptible recording. In addition, bringing magnetized objects into the MSR can cause trapped flux in the SQUIDS which can lead to long and expensive service to fix causing obvious interruptions and scheduling delays. Thus, we have established these guidelines:
- 1. Subjects should not bring any metal objects inside the MSR. Any subject entering the MSR must first “de-metal” (remove any metal objects; empty pockets; remove jewelry, hairclips, pens, clipboards etc.). These include belts, keys, watches, rings/earrings, necklaces, coins, eyeglasses and pieces of clothing with metal parts such as bras with underwires or bras with metal adjustment rings. Non-metallic subject clothing is available in the laboratory upon request.
- 2. No one (not subjects / nor MEG Users) should bring electrical equipment inside the MSR. Objects such as cell phones, pagers, cameras, flashlights, or any other electrical equipment are strictly forbidden.
- 3. Magnets and anything magnetized is never allowed inside the MSR.
- 4. No one should wear shoes inside the MSR. To prevent any metal or magnetic dust from getting into the MSR shoes must be removed before entering the MSR, or shoe covers (provided) should be used.
- 5. Any “unapproved” equipment should not be brought into the MSR. Any “special” equipment must be approved by the director or staff scientist prior to its use.
- 6. Do not use small metal objects (i.e., staples, paper clips) around the MSR.
- 7. NO equipment will be left in the MSR other than the equipment that belongs in the MSR.
Scheduling
Scheduling
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- I. Requesting Time -
- 1. Click on Login location near the bottom of the MEG Schedule/Calendar.
- 2. Enter “Username” and “Password”.
- 3. Click on Login.
- 4. On the calendar - Click on the at the day and time desired.
- 5. Enter the “Add Entry” form information –
- a. Investigator’s Name - enter the last name of the PI / last name of the person who is going to run the scan (acquisition computer). For example - BERMAN / J. Mitchell. In this case Dr. Berman is the PI and Judy Mitchell is running the scan.
- b. Description of experiment – provide a simple description
- c. Comments - Use this field to enter any private comments to the MEG Core staff. These notes will not appear in the calendar. DO NOT enter personally identifying information (PII) into the calendar.
- d. Sensor position – Sitting or Supine.
- e. EEG electrodes – indicate whether EEG, EOG, EMG electrodes will be used.
- f. Date
- g. Time - military time.
- h. Duration – indicate how much time needed to complete your study. Please allow enough time for any possible delays (set up / prep time, subject late, equipment malfunction, etc.).
- i. Hold approval – only use holds if your subject needs to get back with you to confirm the appointment. Appointments can only be held for 2-3 days.
- j. Participants – DO NOT ALTER THIS FIELD (should always be admin for MEG staff who are doing the scheduling).
- k. Repeat Type – if a recurring appointment enter here; however, check with Staff Scientist before scheduling any repeats!
- l. Repeat End Date – *for recurring appointments only.
- m. Repeat Day (weekly) - *for recurring appointments only.
- n. Frequency – for recurring appointments only.
- 6. Click on “Save”.
- II. To Edit or Cancel an Appointment –
- a. Click on the login.
- b. Enter User Name and Password.
- c. Click on the entry to be changed (at the point where it gives the little popup detail description).
- d. Click on option: Edit entry, Delete entry, Add to My Calendar, etc.
*Please note: you must be the owner to be able to edit or delete an entry in the schedule.
- III. To Refresh the Calendar –
- 1. Click on My Calendar.
Facility Access Requests
National Institute of Mental Health
|
Subject: |
Date: 3/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- 1. A Facility Access Request (FAF) must be submitted electronically to become a MEG Lab user. The form may be accessed via the MEG Lab website at: https://kurage.nimh.nih.gov/faf/form.html.
- 2. All the requested information must be provided, such as the protocol #, PI’s last name and the name of the person who be in the MEG Lab running the study. In addition, we must have a cell phone number so that we can contact you in an "emergency".
- 3. The username will be the user’s last name as entered on the Facility Access Form (FAF).
- 4. When a Facility Access Request Form is received the accounts administrator will assign an account and issue a temporary password.
- 5. An email notification of the account name and temporary password will be sent to each applicant.
- 6. User accounts may not be shared.
Subject Guidelines
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- 1. Subject Registration
- a. All subjects participating in MEG studies are required to have a valid medical record number (MRN).
- 1. Subject Registration
- b. It will be the responsibility of the principal investigator (PI) to make sure that all outpatients and control subjects have gone through the appropriate registration process and have a valid MRN.
- c. A doctor’s order is not required for an MEG scan but a progress note must be placed in the subject’s chart indicating the nature of the scan performed, the date, time, and protocol number. The patient’s condition and general performance should also be noted. The progress must also be signed by the appropriate personnel. Progress notes are solely the responsibility of the individual investigators.
- 2. Consent Forms
- a. An IRB approved consent form must be signed by all subjects prior to participating in any MEG research study.
- 2. Consent Forms
- b. Investigators are required to satisfy all Clinical Center documentation requirements.
- c. It will be the responsibility of the PI to assure that subjects have signed the appropriate consent form.
- 3. Subject Pre-Screening
- a. Although MEG/EEG poses no known risk to subjects, some subjects will be ruled out for participation in scanning due to factors involving metallic implants or foreign bodies which may prevent obtaining artifact free data.
- 3. Subject Pre-Screening
- b. It will be the responsibility of the PI to pre-screen subjects for the below listed contraindications during the selection process.
- Conditions That Will Rule Out a Subject:
- • Cardiac pacemaker / Cardiac or neural defibrillators
- • Metal fragments in the eyes
- • Metal plates, pins or bolts in head
- • Any magnetic implantation / implantations made from iron (ferrous products)
- Conditions That Will Rule Out a Subject:
- An Additional Consideration Which Will Rule Out a Subject:
- • Head size greater than 60 cm: if a subject’s head is too large to fit in the helmet
- • Weight greater than 300lbs (seated recording) or 250lbs (supine recording)
- An Additional Consideration Which Will Rule Out a Subject:
- 4. Subject Screening
- a. Investigators may use the MEG Screening Questionnaire and/or Handedness Form as a subject evaluation / screening tool.
- 4. Subject Screening
- b. All MEG subjects should be screened for the following items which may cause recording artifacts.
- Conditions That May Rule Out a Subject:
- • Surgical aneurysm clips
- • Shrapnel
- • Neurostimulators
- • Implanted pumps (i.e., Insulin pumps)
- • Steel pins from root canals; a permanent retainer
- • Ear implants (certain cochlear implants)
- • Metal rods, plates or screws in the body or mouth
- • Previous surgery (if metal was left in the body)
- • Hearing aids (should be removed before scanning)
- • Braces (causes severe artifact)
- • Tattoos (may have metallic paint)
- • Piercings (may contain metal)
- Conditions That May Rule Out a Subject:
- Other Considerations Which May Rule Out a Subject:
- • Movement disorders (i.e., ticks, restless legs, etc., any condition that may cause excessive movement)
- • Vision / Hearing problems
- • Problems using response devices
- Other Considerations Which May Rule Out a Subject:
- c. The confidentially of the MEG Subject Screening Questionnaires and Handedness Forms will be the primary responsibility of the study’s principal investigator.
- 5. Subject Instructions
- a. Users/PI’s are responsible for giving subjects instructions prior to any scheduled procedure.
- 5. Subject Instructions
- b. Subjects should be informed not to wear these items:
- • Bras with underwires
- • Makeup/moisturizer/sunscreen of any kind
- • Clothing containing metallic (shiny) threads or glitter
- • Metal on clothing (i.e., metal buttons, snaps or trimming)
- • Hearing aids
- b. Subjects should be informed not to wear these items:
- c. Subjects should be informed that metallic/magnetic items should not be taken into the Magnetically Shielded Room (MSR). These include such items as:
- • Belts
- • Keys
- • Watches
- • Coins
- • Eyeglasses
- • Cell phones
- • Pagers
- • Credit Cards
- • Small metal objects such as hair pins, paper clips, safety pins, etc.
- • Shoes (may have metallic dust particles on them)
- c. Subjects should be informed that metallic/magnetic items should not be taken into the Magnetically Shielded Room (MSR). These include such items as:
- d. It is the responsibility of the PI to inform subjects that if they arrive unprepared i.e., have metallic/magnetic parts on their clothing that cannot be easily removed, they may be asked to change into non-magnetic clothing which will be provided by staff.
- e. If there is any question about whether an object is magnetic, the object is not taken inside the MSR.
MEG / EEG Setup Procedures
MEG Setup / Fiducial Coil Placement Procedures
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- 1. Head Size / Fit Test
- a. Determine head size by measuring the subject’s head. The Gantry head limits are:
- 1. Head Size / Fit Test
Nasion-Inion Preauricular Point to
Preauricular PointCircumference < 40 cm < 40 cm < 59 cm
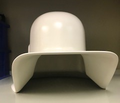
- b. Determine fit by placing the MEG helmet along with a protective cap over the subject’s head.
-
MEG Sizing Helmet-front
-
MEG Sizing Helmet-side
-
- 2. Fiducial Points/Head Coil Placements
- a. If subject has had previous digital pictures of the fiducial points retrieve images and match placement.
- b. A document with images of suggested placement is available here:
- c. Place a small black dot near the nasion (indentation between the forehead and the nose); between the eyebrows midline.
- d. Place a small black dot at the left and right preauricular points centered (about 1.5Cm) in front of the tragus. This should be measured on a straight line from the tip of the tragus to the outer canthus for accuracy.
- e. Take a digital picture of these locations, download and print Place in subject’s MEG file for future reference.
- f. Attach a small (MEG) Adhesive Washers to each head localization coil.
- g. Attach head localization coils at the fiducial marks. Make sure the marks line up with the center of the head coils.
- h. Place tape over the coil and the cable to secure.
- MEG HEAD COIL PLACEMENTS
RIGHT
PRE-AURICULAR POINTNASION LEFT
PRE-AURICULAR POINTRed Yellow Blue
References:
- 1. NIMH MEG Core Facility Data Tutorial Manual
- 2. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc.
EEG Easy Cap Setup Procedures
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
- Procedure:
- A. Head Size / Fit Test
- 1. Determine head size by measuring the subject’s head.
- A. Head Size / Fit Test
- 2. Select cap size: Small (< 56 cm); Medium (< 58 cm); Large (< 60cm).
- 3. Determine MEG gantry fit by placing the MEG sizing helmet along with a protective cap over the subject’s head.
- B. Measuring & Marking Head
- 1. Measure and mark FP1, FP2, FPz and Cz.
- B. Measuring & Marking Head
- C. Mounting the Cap
- 1. Rotate the adaptors in cap so that the narrow opening is toward the back of the head.
- 2. Place anchoring adhesive washer on Fp1 & Fp2.
- 3. Press Fp1 & Fp2 onto adhesive washers. Have subject hold Fp1 & Fp2 in place while turning cap over the head. Gently pull cap over the head and ears into place.
- 4. Check and adjust cap so that the Cz electrode is at the Cz mark.
- 5. Check Fp1 & FP2 and O1 & O2 to assure that they are placed correctly, if not choose another cap size.
- 6. Anchor the cap either with the chest belt or the chin strap.
- 7. Snap electrodes into the adaptors in a systematic manner starting at the back of the head. Insert so that the lead wire points towards the narrow side of the adaptor.
- 8. Push electrode into the adaptor with the fingers or with the aid of an old ballpoint pen where the mine (point) has been removed. Pay attention not to bend or place excessive pressure on the lead wire where it attaches to the electrode.
Electrode Required for PI owned EEG systems
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- For large electrode arrays the use of an electrode cap system, as provided by the MEG Core Facility, is recommended. However, alternative methods of electrode application may be used. Additionally, electrodes can be glued or pasted to the scalp using various types of electrodes. Because of the different properties of the various metals used for electrodes careful attention should be given to the choice of electrode material. These and other factors need to be considered when choosing electrodes for any MEG/EEG application. Below are the recommendations for electrode selection:
- 1. Silver/Silver-Chloride (Ag/AgCl) electrodes are recommended to take advantage of the DC response of the EEG amplifiers.
- 2. Sintered electrodes are preferred to avoid chloriding the electrodes after every few uses.
- 3. It is recommended that the lead length be at least 1.4 meters (48 inches) to allow the amplifier to be reasonably far away from the MEG sensors.
- 4. The material in the electrodes and associated connectors should be non-magnetic.
- 5. The thickness of the EEG electrode should be minimal to avoid fitting problems in the MEG helmet.
- 6. Electrodes should have the DIN style connector.
Reference:
- 1. CTF MEG System Operation and Technical Reference Manual (P/N 900-0028), VSM MedTech Ltd.
Fudicial Points Digital Images
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Three or four views will be taken: 1) Right tragus fiducial point position; Left tragus fiducial point position; Nasion position (on the forehead between the eyebrows); and 4) subject full view (this picture is optional).
Procedure:
- 1. TURN ON THE POWER
- a. Press the power button.
- 2. FOCUSING AN IMAGE:
- a. To FOCUS / FRAME images (especially when taking close-up-shots) use the SHUTTER BUTTON.
- 2. FOCUSING AN IMAGE:
- b. Frame the picture in the IMAGE DISPLAY (for a close up; with the camera about 12 inches away from the object).
- c. Press the ZOOM IN BUTTON then
- d. Press and hold the SHUTTER BUTTON (large round silver button) halfway down to allow the camera to adjust the focus and exposure, then
- 3. TAKING A PICTURE:
- a. Press the SHUTTER BUTTON all the way down to take the picture.
- 3. TAKING A PICTURE:
- 4. VIEWING IMAGES:
- a. Press the MENU / PLAY button to turn on the image display. The last picture you took or viewed appears on the image display.
- 4. VIEWING IMAGES:
- b. Use the CONTROLLER (OK) to scroll through the images.
- c. After reviewing the images, press the PREVIEW BUTTON to turn off the image display.
- 5. UPLOADING / PRINTING images:
- a. Turn camera OFF.
- 5. UPLOADING / PRINTING images:
- b. Connect the camera via the USB cable to a computer running Windows with the HP camera software (Ebi).
- c. Turn the camera on.
- d. Open the HP Photo Imaging Software by double clicking on the icon on the desktop.
- e. Right click then select "MOUNT VOLUME".
- f. Open the DCIM folder.
- g. Open the FOLDER labelled "152_(number for the current month); Jan=1, Feb=2...
- h. Copy pictures and drag to the appropriate "USER" folder. If you don't have a user folder first create one.
- i. Rename the pictures by date taken (Example, 20151201a, 20151201b, 20151201c, etc.
- j. Deletes all pictures from the Camera - if you delete the pictures from the DCIM Folder this will delete your pictures from the camera.
- k. Right click to UNMOUNT the volume.
- l. Unplug the camera.
- m. Turn off camera.
- n. Log out of the computer.
- 6. PRINTING IMAGES:
- a. Select pictures to be printed.
- b. Right Click then sleect OPEN with --> PhotoPrint. Or Left Click on FILE then --> Select Open with PhotoPrint.
- c. Click on FILE then --> /Select PRINT SETUP.
- d. Select "COLOR" as the printer (the HP Laserjet Printer near the Stimulus Computer).
EEG Impedance Check on the MEG System
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
After the electrodes are attached to the subject’s scalp / electrode cap placed, the electrode impedance(s) will be checked to ensure good contact. The impedances measured should only be used to judge scalp contact and should not be considered a precise measure of actual impedance. Ideal impedances for scalp electrodes typically range from 1-5kohms. Impedances for other non-cerebral electrodes ideally should be < 50kohms.
Procedure:
- 1. Attach electrodes to the scalp / place cap.
- 2. Touch the static discharge button before connecting electrodes or cap connector jig to the amplifier unit. Connect the electrodes or electrode cap to the amplifier unit.
- 3. Launch ACQ - Run the appropriate EEG program.
- 4. Select the EEG Setup Window menu.
- 5. Highlight desired channels.
- 6. Click on CHECK IMPEDANCE.
- a. The results are displayed in the appropriate columns.
- b. To check the impedance of all active EEG channels, press the CTRL key on the keyboard at the same time as clicking on the impedance check button.
- c. Please note: The impedance check requires 3 electrodes: The electrode being measured and at least 2 other electrodes.
- 7. Click OK / EXIT.
Reference:
- 1. Data Acquisition Manual, p/n 900-0006, CTF Systems Inc. (www.ctf.com).
EEG Impedance Check using the Grass Impedance Meter
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
An external impedance check should be performed on all electrodes used for EEG, EOG or EMG using the Grass S88 Impedance Meter. The Grass Impedance Meter measures AC impedance (resistance and capacitance). When two or more electrodes are plugged into the electrode switch positions, all electrodes except the one selected electrode being measured are connected and provide the reference for the one being measured.
To perform an Impedance Check, at least two electrodes are required to be plugged in to the impedance meter.
Procedure:
- 1. The Electrode Selector Switch should be at position 1 - 10.
- 2. Plug the ground electrode (Grd) into electrode jack 1 position.
- 3. Plug the other electrode(s) into the jack positions 2 - 10 in a systematic manner.
- 4. Press the Red ON Button to activate the impedance check. *The power will automatically shutoff after approximately 2 minutes. (There is no OFF button.)
- 5. If the impedance is too high:
- a. Take a cotton tip swab dipped in Nuprep (Abralyt or other skin prep) and twirl against the skin.
- b. Re-insert electrolyte.
- c. Re-measure impedance.
- d. Repeat this process until all impedances are within acceptable levels.
- 5. If the impedance is too high:
- Impedance Recommendations
EEG Electrodes 5-10K ohms EMG Electrodes (EOG, ECG, etc.) < 50K ohms
- 6. If the impedance exceeds 199.9K ohm, a “1” will appear in the left display window with all other digits blanked out indicating that the impedance is too high to be read:
- a. Take a cotton tip swab dipped in Nuprep (Abralyt or other skin prep) and twirl against the skin.
- b. Re-insert electrolyte.
- c. Re-measure impedance.
- d. Repeat this process until all impedances are within acceptable levels.
- 6. If the impedance exceeds 199.9K ohm, a “1” will appear in the left display window with all other digits blanked out indicating that the impedance is too high to be read:
Reference:
1. Grass EZM Electrode Impedance Meter Instructions Manual, Grass Instrument Division, Astro-Med, Inc.
Magnetically Shielded Room (MSR) & Subject Support
Magnetically Shielded Room (MSR)
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
I. MSR Room Lighting
- Turning on the lights in the MSR:
- Depress the square green button on the VAC Power Supply Unit which is located on the bottom shelf of the equipment stand outside the MSR.
- Dimming the lights in the MSR:
- Use the Brightness (black) knob to dim the light.
- Turning on the lights in the MSR:
II. MSR Door Operation
- Closing the Door:
- 1. Push the door up to the door frame as far as possible.
- 2. Press the OPEN/CLOSE BUTTON (Black Button) until the air locks activate and the door begins to close then quickly release the button to seal the door.
- Closing the Door:
- Opening the Door:
- 1. Press the OPEN/CLOSE BUTTON (Black Button) until the air locks release and the door begins to open then quickly release the button.
- 2. Pull the door open.
- Opening the Door:
- Door Emergency Operation:
- 1. Emergency Door Open Button - If the door fails to open, press the EMERGENCY OFF BUTTON (red button) located on the wall outside of the MSR. There is also an EMERGENCY OFF BUTTON located on the inside of the MSR door.
- 2. Emergency Door Open Key - If the door fails to open when using the Emergency Off Button, then insert the EMERGENCY DOOR KEY in the upper and lower Emergency Unlock (yellow) keyholes and turn. This will manually release the door locks. Keys and keyholes are located on both sides of the MSR door.
- Door Emergency Operation:
III. MSR Monitors
- A. Oxygen Monitor
- The Safetnet Oxygen Monitor which is mounted in the MEG Lab on the wall just outside the MSR measures the percentage of oxygen in the MEG lab which may be an indication of the air exchange in the MSR and/or the general integrity of the Dewar and related equipment. Refer to Policy No. 10.15 Daily System Monitors / Quality Assurance.
- B. He Gas Flow Meter
- The Gilmont Gas Flow Meter is located inside the MSR mounted on the back left wall. It monitors the MEG Dewar helium level or rate of Helium boil off which gives an indication of the general integrity of the MEG Dewar and related equipment. Refer to Policy No. 10.15 Daily System Monitors / Quality Assurance.
- C. Liquid Helium Level
- The AMI Model 135 Liquid Helium Level Monitor which is located on the stand just outside the MSR measures the amount of helium inside the MEG Dewar. Refer to Policy No. 10.15 Daily System Monitors / Quality Assurance.
References:
- 1. VacuumSchmelze.
- 2. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
Gantry Operation
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
There are two Gantry controls which are located on the side of the Gantry base: 1) the Brake Lever and, 2) the Tilt Control Lever. The Gantry controls have been designed so that the operator is required to use two hands to operate.
- Please note:
- • The Brake Lever and the Tilt Control Lever must be engaged more-or-less at the same time.
- Please note:
- • Pulling up on the Brake Lever turns on the power and releases the brake.
- • Releasing the Brake Lever engages the lock and turns off the power.
- • The Tilt Control Lever is OFF when in the center position.
To re-position / move the Gantry - lift the Brake Lever and hold it in the up position then:
- 1. If raising the gantry,
- a. While still holding the Brake Lever in the release (up) position, lift the Tilt Control Lever handle until the brake is released. You might hear a click or feel the pressure release. Maintain this position until the desired angle of tilt is reached.
- b. As the Tilt Control Lever handle is lifted further the gantry will begin to rise faster.
- c. When the angle of tilt is reached first release the Tilt Control Lever and then release the Brake Lever.
- 2. If lowering the gantry,
- a. While still holding the Brake Lever in the release (up) position, lift the Tilt Control Lever handle to raise the gantry up a few degrees until you hear the click or the Dewar begins to move in the upward direction. This action will release the brake then allow the gantry to lower.
- b. Then push the Lever in the downward direction. Pushing the Tilt Control Lever handle down will cause the gantry to lower.
- 4. Returning the Tilt Control Lever to the center “OFF” position will cause the gantry motion to slow to a stop.
- 5. Release the brake lever allowing it to go back to the horizontal position to turn off the power and engage / lock the brake.
- 6. Never operate the gantry when a subject is seated in the chair or on the bed.
- Gantry Recording Positions
Sitting Position 15 degrees Supine Position 90 degrees Reclined Position at various degrees of tilt
References:
- 1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
Chair Operation
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- Please Note: Chair Weight Limit - The MEG chair can accommodate subjects who weigh up to approximately 300 lbs.
The MEG Chair Height can be raised and lowered for optimal positioning of the subject in the gantry. The chair is a pneumatic-hydraulic unit and there may be a 2-3 second delay when turning controls from the unlocked to the locked position or when making chair adjustments.
- Turn the hand wheel and valves slowly when making any adjustments to allow the air pressure to equalize.
- The Chair Back Rest Tilt can be adjusted for various angles of reclined recording. And, the gantry angle can be adjusted for various angles of reclined recording, however, when the chair is in the upright position the gantry should be at 15 degrees.
- The operator should be completely familiar with the operation of the controls before operating the chair with a subject or patient’s head inside the gantry.
- There are two kinds of controls:
- -The Hand Wheel which controls the directions and rate of movement and
- -The Valve Lock controls which adjustment is selected or activated; it locks and unlocks the Back Rest and the Height controls.
- 1. CHAIR BACKREST ADJUSTMENT
- The TILT Valve Lock - is located on the front panel of the armrest near the top, locks and unlocks the tilt function of the chair backrest.
- 1. CHAIR BACKREST ADJUSTMENT
- a. Slowly turn the TILT Lock Valve to the unlocked position.
- b. Start in the upright position then adjust of necessary or requested by the subject. Position the backrest to provide the optimal level of neck and back alignment and comfort.
- c. With the TILT Lock Valve in the UNLOCKED position the hand wheel controls the movement of the backrest / the backrest angle. Turn the hand wheel:
- • Clockwise to move the backrest forward.
- • Counter-clockwise for backward motions.
- d. The Lock Valve should always be left in the LOCKED position unless adjustments are being made.
- 2. CHAIR HEIGHT ADJUSTMENT
- The ELEVATION Lock Valve – located on the front panel of the armrest near the bottom, locks and unlocks the height function of the chair.
- 2. CHAIR HEIGHT ADJUSTMENT
- a. Slowly turn the Elevation Lock Valve to the unlocked position. * If this valve is released too fast the chair will “jump” in the direction last activated.
- b. Position the subject so that his/her head is at or near the top of the dewar. Care should always be exercised when adjusting the chair height while a subject is seated under the gentry. *When trying to determine how close to the top of the Dewar the subject is positioned periodically ask the subject to raise himself/herself up in the dewar to determine how much room is remaining. Do not raise the chair while the subject is rising up in the chair. Ask the subject to relax back to whatever is comfortable for them, then adjust the chair to the subject.
- c. Turn the Hand Wheel:
- • Clockwise to make the chair move upward.
- • Counter-clockwise for downward motions.
- c. Turn the Hand Wheel:
- d. Turn the Elevation Lock Valve to locked position unless adjustments are being made.
- e. When lowering the chair leave at least 3 inches in the bellows.
- 3. CHAIR MOVEMENT
- The BRAKE Lock Valve - is located on the side panel. It locks and unlock the brakes for the chair’s back and forward movement on the (plexiglass) track. The brake provides only a light braking effect.
- 3. CHAIR MOVEMENT
- a. Turn the valve to the UNLOCKED position. While it is possible to move the chair with the brake in the LOCKED position this should be avoided as it will cause premature wear to the brake pad.
- b. Physically push the chair back so that the subject’s head is positioned directly under the gantry; the back of the head should at the back of the dewar. Two people are required to move the chair so that the chair glides evenly on the track and is not torqued to one side or the other which might damage or break the track. Move the chair into position with one person pushing from each side of the chair.
- c. After adjusting the chair set the Brake Valve to the LOCKED position to prevent movement of the chair.
- d. When done recording, unlock the Brake Valve to move the chair forward to allow the subject to exit the chair without bumping their head on the Dewar or the Dewar arm.
- Always check to make sure that cables are not on the track before moving the chair.
References:
1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
Bed Operation
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- 1. Please note: The MEG bed can only accommodate subjects who weight up to 250 lbs.
- 2. Lower the Gantry to 90 degree tilt (horizontal position). Gantry Controls are located on the right side of the base. The controls require the operator to use both hands to operate. If either handle is released the gantry motion will stop.
- a. Raise the Brake Control Lever (lower / long handle).
- b. Then raise the Direction Control Lever (upper / shorter handle). This will release the brake.
- c. Then move the Direction Control Lever in the downward direction.
- d. Using the Angle Indicator readout located on the gantry near the front pivot point position, lower the gantry to 90 degrees.
- e. Release the Direction Control Lever to stop the motion. Release the Brake Control Lever.
- 3. Lower the chair and slide the chair forward.
- 4. Recline the chair backrest to approximately a 45 degree tilt.
- 5. Remove the arm rest from the chair.
- 6. The back cushion may be removed or left in place.
- 7. If the top portion of the bed will have its angle adjusted, place the Roller Wheel Assembly and follow the steps below; if not skip to section 7.
- • If the chair back cushion has been left in place, first slide the backrest cushion to its lowest position.
- • Mount the Roller Wheel Assembly to the exposed seat back support plate. *These steps are optional if the bed it is to be used in the flat/horizontal position.
- • If the head end cushion will have its angle adjusted, the cushion lock bolts should be removed from their locked position and stored in the holes I the blocks to which they are tied.
- • The head end cushion of the bed can be adjusted in angles from horizontal to approx. 30 degrees using a link to the adjustable chair backrest.
- 8. Using two people, lift the bed by the ends using the hand grips which are mounted to the under side of the bed. *Lift the bed above the optical cables and any other sensitive equipment.
- 9. Set the bed onto the unpadded armrests of the chair. Align the holes on the bed frame with the holes on the pedestal.
- 10. Insert the four mounting bolts, which are tied to the base of the bed, through the holes in the bed base / pedestal.
- a. All four bolts should be screwed in a couple of turns and
- b. Fully tightened when all four are engaged.
- 11. Raise the bed so that it is level with the Dewar.
- 12. Slide the bed back so that it rests against the Dewar.
- 13. For subject safety one side rail must be in place before allowing a subject to get onto the bed; place the second rail after the subject has mounted the bed.
References: 1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com.)
Stimulus / Response / Monitoring Equipment
Stimulus Computer
National Institute of Mental Health
|
Subject: |
Date: 08/18
|
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- Please see MEG Core Facility Staff for training in the operation of the Stimulus computer. Users should not attempt to modify the stimulus computer in any way. If users need additional software, or a software upgrade, please inform MEG Core Facility Staff.
DLP Projector
National Institute of Mental Health
|
Subject: |
Date: 5/18 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- The ProPixx DLP Back Projector system consists of a projector and a screen mounted to the gantry. Images are projected through a hole in the shielded room wall into a set of mirrors which projects the image onto the screen.
- Features:
- -The image size is up to 40 degrees visual field for eye-screen distance of 37.2 to 52.5 cm.
- -a native resolution of 1920 x 1080 and can be driven with refresh rates up to 500Hz (RGB mode) or 1440 Hz (Greyscale mode) with deterministic timing.
- -Uses high brightness LEDs as a light source, giving a larger color gamut
- -The LEDs support high bit depth and high frequency full color stimulation.
- -TACHISTOSCOPC stimulation capability.
- Equipped with:
- -a complete digital I/O subsystem that synchronizes subject I/Os to video refresh with microsecond precision.
- -High-contrast white screen for precision color operation.
- I. Powering the Projector:
- *The Projector has a 30-40 ms delay before it displays an image.
- II. Positioning the Projector:
- The position of the projector does not need to be changed. For further information or help see MEG Staff.
- III. Lens Adjustments:
- Manual Adjustment
- To Focus - Turn the knurled ring (the silver and black lens collar) at the outer end of the lens to adjust the focus until the image is sharp. Generally, the focus should not have to be adjusted.
- Manual Adjustment
- To Zoom - Turn the smooth ring on the lens, closest to the case, to adjust the zoom so that the image fills the screen.
- *The projector lens should be centered in the middle of the screen and should be perpendicular to the mirror; otherwise the image will be distorted, making viewing difficult.
- IV. Program Adjustment:
- All functions, like resolution, can be changed from the desktop of the stimulus computer. However, if changes are made, please change back to the default settings when done.
- V. The Remote Controller:
- The Remote control has a 40 degree reception angle. The Remote must be pointed at the projector's LED (which is located in the back left corner of the projector) within that 40 degree angle to be received.
- Using The Remote To Power The Projector On - Press POWER ON on the Remote Control to switch the projector ON.
- Using The Remote To Power The Projector Off - Press POWER OFF on the Remote Control to switch the projector to OFF / SLEEP mode.
- Please note: The LED ON / OFF button on the remote functions as the shutter on / off button.
- VI. Projector Status Indicators:
- The Projector's LEDs supply info on the power status and the energy status of the projector.
•AWAKE MODE: Press the POWER button and release, the projector will power ON.
The LED will be a solid BLUE light.•SLEEP MODE: Press the POWER button for 3 secs,
the LEDs will be a solid RED.
The projector will be in the sleep mode.
•THERMAL SHUTDOWN: Flashing RED LEDs indicates the lamp is shutting down.
When flashing stops, the projector is in the SLEEP Mode (OFF)
as indicated by the solid RED LEDs.
- VII. Reversing The Projection Scheme For Supine Recording – To Be Determined
- a. Press MENU.
- b. Use OPTION2 menu
- c. Select REAR projection- choose this option if pictures are projected from the rear of a reflective screen.
- d. Select CEILING mount – choose this option if the projector is installed on the ceiling (or upside down).
- VII. Reversing The Projection Scheme For Supine Recording – To Be Determined
- VIII. Mirror Adjustments
- Wall Mirror Adjustments for Seated Recording:
- 1. Project an image onto the mirror.
- Wall Mirror Adjustments for Seated Recording:
- VIII. Mirror Adjustments
- 2. Adjust the wall mirrors:
- a. Position the top mirror in front of the lens so that the image is reflected down to the bottom mirror.
- 2. Adjust the wall mirrors:
- b. Adjust the bottom mirror so that the image is projected centered onto the screen.
- IX. Ceiling Mirror Adjustments for Supine Recording:
- 1. Place the ancillary wall mirror (smaller mirror) on the 2nd set of wall brackets.
- IX. Ceiling Mirror Adjustments for Supine Recording:
- 2. Position the top mirror so that it projects onto the smaller mirror. Position the smaller mirror so that it projects onto the ceiling mirror.
- 3. Slide the ceiling mirror into position so that the image from the ceiling mirror is projected onto the screen.
- X. Screen Adjustments
- 1. There are two possible viewing screens:
- a. The original screen with the original color pallet and,
- b. At white screen for high-resolution color.
- 1. There are two possible viewing screens:
- 2. Position the screen so that the image is projected centered onto the screen. If possible, the screen should be perpendicular to the floor.
- 3. The screen distance can be increased or decreased by loosening the black knob located on the telescoping screen arm and adjusting the arm length.
- 4. If necessary, the screen can also be removed and flipped so that it is closer to the subject. Loosen the knob located on the telescoping screen arm. Pull the arm out, flip the screen and re-insert. Position the screen and tighten the knob.
- 5. Use the black knob located on the gantry mounting bar to raise and lower the screen.
- 6. If you use the High-Resolution Screen please put the original screen back in place when done.
Reference:
1. Propixx DLP Projector User Manual.
Nerve / Muscle Stimulator
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
The Grass S88 Stimulator is a dual output general purpose stimulator intended for nerve and muscle stimulation procedures. The two output channels can be operated independently or synchronized to produce complex paradigms. The outputs are non-isolated constant voltage positive pulses. Features include computer compatibility and flexibility of synchronization circuits: the synchronous inputs and outputs are TTL, 5 volts, PC compatible. A rear DB25S connector permits external analog control of the timing circuits. The Stimulus Isolation Unit (SIU) allows for applications requiring isolation and/or constant current. Grass S88 Electrical Nerve/Muscle Stimulator - Stimulation is triggered via TTL outputs from the S88 to the MEG system electronics.
- 1. Power Switch
- a. The POWER toggle switch is flanked by the ON pilot lamp and the red overload lamp.
- 1. Power Switch
- b. In the ON position, the pilot lamp will glow orange, indicating that line power is being supplied to the instrument.
- c. The OVERLOAD lamp will glow red in the event of a short circuit at either output. The circuit overload shuts off the HIGH VOLTAGE power supply.
- d. The red indicator lamp will remain ON until the POWER switch is turned OFF for a few seconds.
- 2. Stimulus ON-OFF-ON Lever Switch
- a. The STIMULUS ON-OFF-ON LEVER SWITCH is located at the right-hand corner of each channel.
- 2. Stimulus ON-OFF-ON Lever Switch
- b. The upper ON position is for continuous voltage at the output; the lever switch will remain depressed (in the on position) when released; power will remain ON until the lever is switched to the up or off position.
- c. In the lower ON position the lever switch will remain ON only if it is depressed; it will return to the OFF position as soon as it is released.
- 3. Stimulus Mode
- The S88 FUNCTION can be set to deliver:
- a. Single – the RED SINGLE pushbutton is for manual operation (single independent pulses); also, delivers single repetitive stimulus.
- b. Repeat – repetitive stimulus; continuous presentation of a selected stimulus pattern (recurring pulses).
- c. Trains – trains per seconds (TPS) covers a range of 0.01 to 100 TPS; delivers a select number of pulses in defined intervals/delays.
- d. Twin Pulses – pulse per seconds (PPS); delivers two pulses of identical voltage and duration; the time between the onset of the first and second twin pulse is determined by the DELAY Circuit; twin pulses can be obtained singly, repetitively on in trains of pulses (can be used to determine nerve and muscle refractory times.
- e. Trains of Twin Pulses – delivers two pulses together in a series in defined intervals/delays from its single output.
- 4. Controls
- All controls are equal to the setting on the dial multiplied by the setting indicated on the decade (multiplier) switch.
- a. Rate – determines the rate at which pulses are delivered in pulses per second (1/100 sec to 100 PPS).
- b. Delay – length of time before the pulse starts; pre-pulse interval (10usec to 10 sec).
- c. Duration – pulse length; determines the length of time (T) in milliseconds that a pulse of a given frequency and voltage is delivered [1 msec to 10,000 msec (10 sec)].
- d. Volt Control - Controls the intensity / strength of the pulse; range at the output is from 0.01 to 150 volts. Always begin with the VOLTS dial set to minimum (1) and increase until the desired stimulus intensity is achieved.
- e. Voltage Decade (multiplier) Switch- multiplier switch; the output impedance is also determined from the Volts Decade Switch.
- i. In the first four positions, the output impedance is 250 ohms and is constant at these four positions:
- a. X.01,
- b. X.1,
- c. X1 and
- d. X10(SIU).
- i. In the first four positions, the output impedance is 250 ohms and is constant at these four positions:
- ii. At X10(25Ω) the output impedance is 25 ohms.
- iii. For special applications requiring low impedance, high current output - set the multiplier to X10(25Ω). This position is provided for use with low impedance electrodes to obtain a relatively high current out. When using this mode, caution should be taken since very high stimulus currents can be delivered.
- a. When a Stimulus Isolation Unit (SIU) is connected in series with the output the:
- b. X10(SIU) position is recommended for 15 to 150 volts out; *The SIU7 Isolation /Constant Current Unit should be operated at all times with the stimulator VOLTS multiplier set to the X10(SIU).
- c. X1 position is recommended for outputs of less than 15 volts.
- iii. For special applications requiring low impedance, high current output - set the multiplier to X10(25Ω). This position is provided for use with low impedance electrodes to obtain a relatively high current out. When using this mode, caution should be taken since very high stimulus currents can be delivered.
- e. Train Rate – in the S2 TRAIN position, trains of stimulus patterns are presented at the output of S2 at the rate set by this control.
- f. Train Duration - in the S2 TRAIN position, trains of stimulus patterns are presented at the output of S2 at the duration set by this control.
- g. Train Mode – To obtain trains, this switch must be in the SINGLE or REPEAT position.
Grass S88 Stimulator Specifications Train Rate (S1 and S2) 1/100 sec to 100 TPS (4 decades) Train Duration 1msec to 10 secs (4 decades) Rate (S1 and S2) 1/100 sec to 1000 PPS (5 decades) Pulse Delay (S1 and S2) 10usec to 10 secs (6 decades) Pulse Duration (S1 and S2) 10usec to 10 secs (6 decades) Synchronous Outputs (TTL) S1, S2 S1 Delay, S2 Delay, Train Rear Panel Outputs 1 or 10 msec and Train End Synchronous Inputs (TTL) Train Duration, S1 Delay, S2 Delay, Trigger Rising or Falling edge Rear Connector (DB25S) All SYNC INPUTS and OUTPUTS; Volts Out (S1 and S2) 10mV to 150V (4 decades) Peak Output Current 150mA with 1000Ω on highest range Output Impedance 250Ω nominal on all voltage ranges; 25Ω and 100kΩ on highest range AC Power 115/230V, 50/60Hz, 125 watts peak, 20 watts standby Maximum power output 22 watts Current output 150 milliamperes Output Impedance determined by the position of the VOLTS multiplier switch Tolerance All parameters are accurate to +5%
- 5. Additional Notes
- a. The output is a positive (with respect to chassis ground) non-isolated constant voltage square pulse.
- b. The S88 cannot deliver a true symmetrical biphasic pulse which is equal in positive and negative amplitudes. However, if a Model Stimulus Isolation Unit (SIU)5 is used at either the S1 or S2 output, a biphasic waveform can be produced which, although not symmetrical, does have a negative and positive component which is equal in effective energy in terms of coulombs, if averaged over a sufficiently long period of time.
- c. It is possible to obtain a true symmetrical biphasic pulse by mixing the output pulses from both S1 and S2 outputs through two Stimulus Isolation Units. Polarity can be changed only by connecting the S88 in series with an SIU and reversing polarity at the output of the SIU.
- 5. Additional Notes
Reference:
1. Grass S88 Muscle / Nerve Stimulator Manual
Auditory Stimulus System
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- The auditory stimulus is produced using Presentation or SoundBlaster software. The interface includes: a Stereo amplifier, a pair of low-distortion silicone tubes which have about a 10 msec delay (due to the length of the tubing) and a bandwidth of 5 kHertz, foam ear inserts (in various sizes) to fit in the subject’s ear canal, and a sound level meter to calibrate sound delivered to the subject. Insertion depth affects interaural attenuation. Be sure to select the correct size Foam Ear Tip to obtain the best fit in the ear canal. Insert as far as possible into the ear canal.
- 1. Attach the Foam Ear Tip Insert into the short Auditory Tubing Inserts. A connector (tube nibble) is required to keep the insert from coming out.
- 2. Attach the short Auditory Tubing Inserts onto the end of the Low Distortion Silicone Auditory Tubes which are hanging on each side of the Gantry mounting bar. Place Red on the right side and the Blue on the left.
- 3. Slowly roll (rather than squeeze) the Foam Ear Tip into so that they are as small as possible.
- 4. Quickly insert the compressed plug well into the ear canal.
- 5. Hold in the ear with finger tip until expansion is complete.
- 6. Repeat process for the remaining ear.
- 7. The tubing may be taped to the ear or on the subject’s cheek to assure that the insert does not become dislodged during testing.
- 8. Click on Presentation or SoundBlaster software from the desktop on the Stimulus Computer located at the operator’s console.
- 9. Test to make sure that the equipment is working properly and to assure that the sounds are being delivered to both left and right ears.
- 10. Adjust the sound intensity to the desired level (dB).
How To Place Foam Ear Tip Inserts
For A Secure & Comfortable Fit1. Roll the tube really tight (usually better if you use both hands). 2. Figure out how the tube should go in the ear canal first by determining
the angle of the ear canal. Generally, the ear canal goes up at an angle.3. Pull the ear out and up to open up the canal. 4. Then gently push the tube in so that it is situated behind the tragus. 5. Hold the tube in place for several seconds to allow the tube to expand in the ear canal.
*If you do not hold the tube in place while it expands it is possible that it might be push out
of the ear canal while expanding.Note: if the tube does not go or fit in the ear canal do not force it in; take the tube back out and re-roll;
if it still does not fit, use a smaller size.
Eye Tracking System
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- The Infrared Eye Position Tracking System – The infra-red eye tracking system captures a zoomed in video of the subject’s eye after calibration, and can estimate gaze position onto a screen providing gaze coordinates and pupil dilation. Gaze position can then be broadcast to the stimulus and/or ACQ computer for real-time or post-hoc analysis.
- The Infrared Eye Position Tracking System includes the:
- 1. Infrared Camera (located in the MSR).
- 2. Infrared Light
- 3. Eye Tracking Computer
- 4. Eye Tracking Software
Response Devices
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- I. Lumitouch Response Pad
- The Lumitouch is a fiber optic response keypad where there are five response buttons arranged in a row to correspond to the thumb and the fingers. The response keypads and cabling are fabricated from 100% plastic materials and therefore do not cause electromagnetic interference. The fiber-optic cables run from the pads through a wave guide to a controller box which is connected to the stimulus PC via a USB cable.
- 1. Place the response pad on the left or right arm rest.
- 2. Arrange fingers so that all or a subset of fingers can be used in natural
- order and positioning when responding to visual and/or auditory stimuli.
- 3. Place the cables so that they are not on the MEG chair’s track when the chair is being moved.
- 4. Instruct the subject in the use of the Lumitouch Response Keypad for the research study task.
- II. FORP Response Pad
- The FORP is a Fiber-Optic Response Pad (FORP) where the 4 keys arranged in a diamond pattern. There are 4 colored buttons which are arranged in a diamond pattern: Blue=1, Yellow=2, Green=3, Red=4. The response keypads and cabling are fabricated from 10% plastic materials and therefore do not cause electromagnetic interference. The fiber-optic cables run from the pads through a wave guide to a controller box which is connected to the stimulus PC via a USB cable.
- 1. Instruct the subject to hold or cup the response pad in the dominant or non-dominant hand while using the thumb to respond to the appropriate color, position, number or pattern. Position the pad so that the cable is in the superior orientation.
- 2. Place the cables so that they are not on the MEG chair’s track when the chair is being moved.
- 3. Instruct the subject in the use of the FORP Response Pad for the research study task.
- III. Joy Stick Control
- The Joy Stick is a manual input device with a moveable control lever that can be tilted in various directions to control pointing devices or on-screen objects used for graphic applications.
- 1. Instruct the subject to grasp the joystick control lever.
- 2. Place the cables so that they are not on the MEG chair’s track when the chair is being moved.
- 3. Instruct the subject in the use of the joystick for the research study task.
- IV. Motion Detector
- The laser Motion Detector is a device that contains a physical mechanism or electronic sensor that quantifies movement which is integrated with or connected to other devices that alert the user of the presence of a moving object within the field of view.
- V. Optical Microphone
- An Optical Microphone is an acoustic-to-electric transducer or sensor that converts sound into an electrical signal.
- VI. Pneumatic Air Pressure Device
- The Pneumatic Air Pressure Device is attached to the pressure response ball which the subject squeezes to indicate a response. The unit can be calibrated for a gradated response or the thresholds can be set to give an on / off response.
Stimulus Devices
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
response input, subject reaction and / or response time.
Procedure:
- I. Air Puff Stimulator
- The Air Puff Stimulator is a tactile sensory nerve stimulator. The Air-puff stimulator is applied to the fingertip. It produces a puff of air which provides tactile stimulation that produces a measurable sensory response in the nerve and sensorimotor cortex.
- II. LED Flasher
- The LED Flasher is a light emitting diode which flashes a red strobe light for visual system stimulation.
- III. Piezo Buzzer
- A buzzer device which has no moving parts which uses the electromechanical interaction between the mechanical and the electrical state in a crystalline material to measure pressure, acceleration, strain or force and converts them to an electrical charge.
Voice Intercom System
National Institute of Mental Health
|
Subject: |
Date: 11/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- I. The Voice Intercom System consists of:
- 1. The Intercom Electronics Box - located at the acquisition workstation / operator’s console. The Intercom Electronics Box allows the MEG operator to adjust the volume level at the console and the volume level inside the MSR independently. When at the Acquisition Console, the MEG operator can communicate with the subject inside the MSR through this device. This system works like a Walkie-Talkie, that is, when the operator is talking (depressing the “talk” button he/she cannot hear the subject and when he/she releases the button he/she can hear the subject speaking).
- I. The Voice Intercom System consists of:
- 2. Parabolic Microphone - located inside the MSR. It is used to pick up and amplify the subject’s voice so that it can be heard at the operator’s console in order to facilitate communication between the subject and the operator.
- 3. Flat Speaker - located inside the MSR. It is used to pick up and amplify the operator’s voice so that it can be heard by the subject inside the MSR.
- 4. There are no intercom controls inside the MSR.
- II. Operation:
- 1. Press the Red power button to turn ON the Intercom Electronics Box.
- II. Operation:
- 2. Press the PUSH TO TALK button located on the front of the Intercom Electronics Box to speak to a subject inside the MSR.
- 3. Release the button to hear the subject speak.
- 4. Adjust the volume inside the MSR, so that the subject inside the MSR can hear the operator, using the knob labelled “MSR” located on the Intercom Electronics Box.
- 5. Adjust the volume at the Acquisition Workstation / Operator’s Console, so that the operator at the console can hear the subject, using the knob labelled “Console” on the Intercom Electronics Box.
Reference:
- 1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
Video Display Monitor
National Institute of Mental Health
|
Subject: |
Date: 11/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- *Always monitor subjects via the Video Display Monitor when running a study.
- THE SUBJECT MUST BE OBSERVED AT ALL TIMES DURING TESTING.
- The Video Display Monitor which is located at the acquisition workstation / operator’s console is used to monitor subjects inside the MSR. MEG users will observe the subject at all times while inside the MSR. There are currently two channels / two cameras in use for subject observation. Each camera is located or mounted at a different angle. Select the camera angle that is best for viewing the subject and any related equipment.
- a. To turn the monitor on - press the ON/OFF switch located on the front panel of the Video Display Monitor.
- b. Press the channel button once to access the next channel.
- c. Continue to press the channel button to access the other channels.
Channel 1 Camera 1 (Infrared Camera) Channel 2 Camera 2 (Color Camera)
Infrared Lighting
National Institute of Mental Health
|
Subject: |
Date: 11/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
'Procedure:
- 1. The Infrared Light illuminates the inside of the MSR when recording in a dark environment so that the subject may be seen via the Video Display Monitor. The Infrared Light Control Box is located on the stand outside the MSR.
- 2. Press the Red ON/OFF switch to turn the power on and off for the Infrared Light Power Supply (SEC 1212).
Data Acquisition
Data Acquisition
National Institute of Mental Health
|
Subject: |
Date: 10/03
|
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- The Acquisition Computer controls all aspects of electronics, tuning, aquisition and data storage. The Acquisition Computer is configured with CTF's Omega software. Users are prohibited from attempting to alter the Acquisition computer setup in any way, and should not access any maintenance functions. Please see MEG Core staff for training in operating the Acq computer.
Infection Prevention / Control
Infection Control / Universal Precautions
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedures
- I. Standard / Universal Precautions include these practices:
- 1. Hand Hygiene – See Hand Hygiene, Cleaning & Washing Procedures
- 2. Use of protective barriers / personal protective equipment (PPE), which will include:
- a. Gloves - (latex or latex-free non-sterile gloves)
- i. During EEG/ EMG / Evoked Fields set up and clean up;
- ii. When abrading the skin;
- iii. When applying, handling and processing electrodes;
- iv. When hands are likely to be contaminated with blood, body fluids, secretions or excretions;
- v. When handling any equipment that comes in contact with subjects with a known infection.
- a. Gloves - (latex or latex-free non-sterile gloves)
- 2. Use of protective barriers / personal protective equipment (PPE), which will include:
- b. Gowns / Plastic apron –
- i. Usually not indicated for routine MEG Scans;
- ii. To be worn during activities that are likely to generate splashes.
- b. Gowns / Plastic apron –
- c. Masks –
- i. Usually not indicated for routine MEG scans;
- ii. To be worn wherever splashes, spray, spatter or droplets may be generated toward the eyes, nose or mouth (in these situations wear a mask and eye protection or a chin length face shield).
- c. Masks –
- d. Protective Eyewear (i.e., eye shields or goggles) –
- i. Usually not indicated routine MEG scans;
- ii. To be worn wherever splashes, spray, spatter or droplets may be generated toward the eyes, nose or mouth (in these situations wear a mask and eye protection or a chin length face shield).
- d. Protective Eyewear (i.e., eye shields or goggles) –
- 3. Appropriate handling and disposal of sharps and other contaminated or infectious waste –
- a. All sharp items including needles and blunted needle tips will be disposed of in a Sharps Container.
- b. Sharps container will be disposed of when ¾ full; seal container closed and place in a Medical Pathological Waste (MPW) box.
- c. All disposable items contaminated with blood, body fluids, secretions or excretions will be disposed of in a MPW box.
- 3. Appropriate handling and disposal of sharps and other contaminated or infectious waste –
- 4. Use of Aseptic techniques- to control microorganisms in the environment-
- a. Cleaning – removal of all foreign materials using isopropyl alcohol (i.e., soil, organic material) from objects. Cleaning must precede disinfection and sterilization procedures.
- b. Decontamination – using Dispatch (1:10 solution of Sodium Hypochlorite) renders instrument surfaces safe to handle by reducing microbial burden.
- c. Disinfection – items are sent to Central Sterile Supply where a chemical or physical agent is used to eliminate nearly all recognized pathogenic organisms but not necessarily all microbial forms on inanimate objects.
- 4. Use of Aseptic techniques- to control microorganisms in the environment-
- 5. Use of Sterilization – items are sent to Central Sterile Supply where:
- a. Gas is used to eliminate or destroy all forms of microbial life, especially microorganisms and spores.
- 5. Use of Sterilization – items are sent to Central Sterile Supply where:
- II. Transmission Based Precautions – additional precautions which are designed to interrupt transmission of known infections which should be used in addition to Standard / Universal Precautions when transmission of known infections might not be contained by using Universal Precautions alone. Transmission based precautions are based upon and used for patients known or suspected to be infected or colonized with epidemiologically important or highly transmissible pathogens that can cause infections:
- 1. Respiratory Precautions –
- a. Airborne Transmission (i.e., tuberculosis, measles virus, chickenpox virus);
- b. Acid Fast Bacilli (AFB) (i.e., tuberculosis) or
- c. Droplet Transmission (i.e., mumps, rubella, pertussis, influenza);
- 1. Respiratory Precautions –
- 2. Contact Precautions - Direct or Indirect Contact dry skin (i.e., colonization with Multi-Resistant Staphylococcus Aureus [MRSA], ringworm, head lice, scabies) or
- 3. Strict Precautions - Any combination of these routes. *See IC Flipchart.
- 4. CNS Precautions – contact with blood or body fluids especially cerebral spinal fluid (CSF).
References:
- 1. National Institute of Health, Clinical Center Hospital Epidemiology Service (HES); http://intranet.cc.nih.gov/hospitalepidemiology/ .
- 2. OSHA Infections Control Guidelines; https://www.osha.gov/SLTC/healthcarefacilities/infectious_diseases.html.
- 3. CDC Infections Control Guidelines; https://www.cdc.gov/hicpac/pdf/core-practices.pdf .
Hand Hygiene, Cleaning & Washing Procedures
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
subject /patient to staff.
Procedure:
- I. Steps to Assure Effective Hand Hygiene:
- a. Keep nails short and neat. Cracked or chipped nail polish provides crevices for organisms.
- I. Steps to Assure Effective Hand Hygiene:
- b. Limit wearing of hand and wrist jewelry. Jewelry provides crevices for organisms.
- c. Dry, cracked, broken skin increases chance of harboring transient bacteria. Dry hands well. Do not over use antimicrobials. Use hand lotion.
- d. Liquid soap from a dispenser is preferred, however, if bar soap is used, rinse soap after use and keep on racks that allow drainage of water.
- II. What to Use for Hand Hygiene:
- 1. Antimicrobial Soap and Water
- Hands must be washed using an antimicrobial soap (Bactifoam) and running water.
In the absence of a true emergency, personnel should always wash their hands with soap and water.
If hands are visibly soiled they must be washed using an antimicrobial soap and running water as soon as possible.
- Hands must be washed using an antimicrobial soap (Bactifoam) and running water.
- 1. Antimicrobial Soap and Water
- II. What to Use for Hand Hygiene:
- 2. Alcohol Based Gels
- If hand washing using soap and running water is not possible an alcohol gel such as Avagard D (61% alcohol) may be used.
Alcohol gel products do not require water.
- If hand washing using soap and running water is not possible an alcohol gel such as Avagard D (61% alcohol) may be used.
- 2. Alcohol Based Gels
- III. How to Wash Hands:
- a. Use continuously running water.
- III. How to Wash Hands:
- b. Wet hands thoroughly.
- c. Dispense enough hand soap for a good lather.
- d. Vigorously rub together all surfaces of lathered hands for at least 10 seconds.
Take care not to break or abrade your skin.
- d. Vigorously rub together all surfaces of lathered hands for at least 10 seconds.
- e. Keep hands down at all times so run off goes into sink and not down arms.
Avoid splashing.
- e. Keep hands down at all times so run off goes into sink and not down arms.
- f. Rinse thoroughly under a stream of water.
- g. Dry hands well with paper towel.
- h. After washing turn off hand operated faucets with clean dry paper towel and
dispose of properly.
- h. After washing turn off hand operated faucets with clean dry paper towel and
- IV. How to Clean Hands Using Alcohol Based Gels:
- a. Apply to dry hands.
- IV. How to Clean Hands Using Alcohol Based Gels:
- b. Apply enough to moisten all hand surfaces (front and back).
- c. Rub hand together for 20 seconds; cover all surfaces of the hands,
fingers and nails.
- c. Rub hand together for 20 seconds; cover all surfaces of the hands,
- d. Allow hands to dry.
- e. Do not wipe off excess gel; rub on skin until dry.
- f. After every 10 applications of hand gel, perform hand hygiene with soap and running water.
- g. If hands are visibly soiled they must be washed using soap and water.
- V. When to Clean Hands:
- • At reporting to work (at the beginning of your shift);
- V. When to Clean Hands:
- • At the beginning and end of each MEG scan;
- • Before and after subject/patient contact;
- • Before and after touching high risk subjects or patients
(before taking care of a particularly susceptible patient – i.e., severely immuno-compromised).
- • Before and after touching high risk subjects or patients
- • After contact with blood or other body fluids, secretions, or excretions.
- • Before donning gloves;
- • After removing gloves- gloves can become perforated during use;
bacteria can multiply rapidly on gloved hands.
- • After removing gloves- gloves can become perforated during use;
- • After touching objects that are likely to be contaminated with microorganisms
(e.g., equipment or other items, keyboards, telephones, doorknobs, stair banister, etc.
- • After touching objects that are likely to be contaminated with microorganisms
- • After applying or adjusting electrodes.
- • After removing electrodes and cleaning hair and scalp.
- • After handling electrodes for cleaning or after disinfecting.
- • Before and after eating.
- • Whenever hands are soiled;
- • After going to the bathroom.
- • After blowing or wiping nose, coughing or sneezing.
References:
- 1. Refer to the CC Handwashing Policy.
- 2. National Institute of Health, Clinical Center Hospital Epidemiology Service (HES); http://intranet.cc.nih.gov/hospitalepidemiology/ .
- 3. OSHA Infection Control Guidelines; www.osha.gov
- 4. CDC Infection Control Guidelines: www.cdc.gov
Cleaning, Disinfection & Sterilization of MEG Equipment
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
I. Personal / Workspace Protections
- 1. Gloves will be used when:
- a. Abrading skin,
- b. Cleaning, disinfecting or handling equipment used on abraded skin,
- c. Handling all soiled instruments and equipment,
- d. In contact with a patient/subject with a known infectious disease,
- e. In accordance with Universal / Standard Precautions, Transmission Based Precautions and CC Infection Control guidelines.
- 1. Gloves will be used when:
- 2. Workspace Protective Impervious Barrier are used: -
- a. To cover the work area when abrading the skin to place “contaminated/used” equipment or supplies.
- b. When temporarily maintaining any item considered contaminated if needed for additional use,
- c. To place all soiled instruments and equipment,
- d. To place items that have come in contact with a patient/subject with a known infectious disease,
- e. In accordance with Universal / Standard Precautions, Transmission Based Precautions and CC Infection Control guidelines.
- 2. Workspace Protective Impervious Barrier are used: -
II. Non-portable non-disposable / reusable equipment
- 1. Routine Cleaning Procedure
- a. All Non-Disposable Immobile or Non-Immersable equipment that comes in contact with a subject/patient will be routinely cleaned by the person(s) conducting the MEG scan using a hospital approved disinfectant such as Hydrogen Peroxide, 70-90% ethyl alcohol or isopropyl alcohol after each subject/patient use.
- 1. Routine Cleaning Procedure
Materials Required: Gloves, a hospital approved disinfectant such as Hydrogen Peroxide, 70-90% ethyl or,/isopropyl alcohol. Responsibility: Each User Frequency: After each use.
- 2. Known Infectious Disease Procedure
- a. Most EEG/MEG equipment (other than electrodes and caps) usually poses no significant hazard of infection transmission, however, when used by a patient with a known infectious disease the equipment will be disinfected in compliance with Transmission Based Precautions by each User after each subject/patient use.
- 2. Known Infectious Disease Procedure
Materials Required: Gloves, Prepping (Blue) Pad, Disposable Wash Cloth, a hospital approved disinfectant
such as Hydrogen Peroxide, 70-90% ethyl or,/isopropyl alcohol.Responsibility: Each User Frequency: After each use.
III. Portable non-disposable / reusable equipment
- 1. Routine procedure for equipment used on abraded skin:
- a. All portable non-disposable equipment used on abraded skin will be treated as in Infection Control - EEG Caps & Electrodes
- 1. Routine procedure for equipment used on abraded skin:
- 2. Routine Procedure for equipment used on un-abraded skin
- a. All Portable Non-Disposable equipment, i.e., head localization coils, that comes in contact with un-abraded and otherwise intact skin (including sweat) will be cleaned using a hospital approved disinfectant such as Hydrogen Peroxide, 70-90% ethyl alcohol or isopropyl alcohol.
- 2. Routine Procedure for equipment used on un-abraded skin
Materials Required: 70-90% Ethyl Alcohol, Isopropyl Alcohol, Alcohol Prep Pads, and gloves Responsibility: Each User Frequency: After each use Transport to CHS: MEG Staff
- Procedure:
- i. Wash hands.
- ii. Wipe the Head Localization Coils with alcohol.
- iii. Adhesive Remover may be used occasionally to remove any adhesive buildup or sticky residue.
- iv. Wash hands.
- Procedure:
- 3. Known Infectious Disease (Abraded Skin or Un-Abraded Skin)
- a. All Portable Non-Disposable / Reusable Equipment used by a patient with a known infectious disease will treated as equipment used on abraded skin (Infection Control - EEG Caps & Electrodes) and be sent to CHS for disinfection /sterilization.
- 3. Known Infectious Disease (Abraded Skin or Un-Abraded Skin)
IV. Disposable / single use equipment
- 1. Routine Procedure for Single Use Equipment used on Abraded or Un-abraded Skin
- a. All Disposable / Single Use Equipment used abraded skin will be disposed of in the trash. Gloves will be used when abrading the skin.
- 1. Routine Procedure for Single Use Equipment used on Abraded or Un-abraded Skin
- 2. Known Infectious Disease (Single Use Equipment)
- b. All Disposable / Single Use Equipment used by a patient with a known infectious disease must be disposed of in a Medical Pathological Waste (MPW) Box.
- 2. Known Infectious Disease (Single Use Equipment)
V. Adverse Occurrences:
- 1. Course of Action for Adverse Occurrence / Exposure to an infectious agent.
- a. Follow the Clinical Center Infection Control Guidelines in accordance with the specific kind of exposure.
- b. Report to Occupational Medical Service (OMS).
- c. Fill out a MEG Problem Report form.
References:
- 1. National Institute of Health, Clinical Center Hospital Epidemiology Service: http://intranet.cc.nih.gov/hospitalepidemiology/ .
- 2. OSHA Infection Control Guidelines: www.osha.gov
- 3. CDC Infection Control Guidelines; www.cdc.gov
Infection Control - EEG Caps & Electrodes
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
Materials Required: Gloves, Prepping (Blue Pad), Disposable Wash Cloth, Biohazard Transport Container,
Zip Lock Specimen Bag (2), Steam / Gas Sterilization Request Form,
Contents/ Warning Label, Marker, MPW Box, and a hospital approved
disinfectant such as Hydrogen Peroxide, 70-90% ethyl or isopropyl alcohol.Responsibility: Each User / Research Assistant Frequency: After each use Transport to CHS: MEG Staff
- I. Non-Disposable Electrodes(s) – e.g., Silver/Silver Chloride Disc Electrodes, Gereonics Silver /Silver Chloride Electrodes, Grass Gold Electrodes
- 1. Latex rubber gloves must be use whenever handling and/or processing electrodes used on abraded skin. For individuals sensitive to latex, nitrile rubber gloves may be used.
- 2. Place the disk end of the electrode in the zippered section of the 2-pocket zip lock plastic bag.
- 3. Place the wire end in the un-zippered pocket of the zip lock plastic bag.
- 4. Place the plastic bag containing the “contaminated” electrode(s) in the top tray of the three (3) piece amber OSHA approved Biohazard Container.
- 5. Place the lid on the Biohazard Container.
- 6. Place the Biohazard Container on the top shelf of the Environmental Services Department (ESD) Processing Cart.
- 7. Fill out a “Steam/Gas Sterilization Request Form” for each container and place the form on the top of the appropriate closed Biohazard Container.
- 8. MEG staff will transport the Biohazard Container to ESD for disinfection/sterilization.
- 9. Biohazard Containers with “contaminated” equipment will be logged in and out per ESD procedures.
- II. Non-disposable EEG Cap – e.g., Easy Cap
- 1. Latex rubber gloves must be used whenever handling and/or processing an EEG Cap that has been used on abraded skin. For individuals sensitive to latex, nitrile rubber gloves may be used.
- 2. Removed all electrodes from the cap. *The EEG Cap and electrodes will be processed separately.
- 3. Place the cap in the top tray of the three (3) piece amber OSHA approved Biohazard Container.
- 4. Place the lid on the Biohazard Container.
- 5. Place the Biohazard Container on the top shelf of the ESD processing cart.
- 6. Fill out the Gas Sterilization Request form and place on top of the appropriate closed container.
- 7. MEG staff will transport the Biohazard Container to ESD for disinfection / sterilization.
References:
- 1. National Institute of Health, Clinical Center Hospital Epidemiology Service (HES); http://intranet.cc.nih.gov/hospitalepidemiology/ .
- 2. OSHA Infections Control Guidelines; www.osha.gov .
- 3. CDC Infections Control Guidelines; www.cdc.gov .
VSM Easycap (Model B-VSM-0123) Electrode & Cap Maintenance, Cleaning & Disinfection
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Procedure:
- After each use in the MEG Lab (B1 D65B) the VSM Easycap and electrodes will be transported in a Biohazard Transport Container to the NINDS EEG Department (10 / CRC Rm 7-3753) by the NINDS EEG Department staff to be cleaned and disinfected as outlined below.
Materials Required: Gloves, Biohazard Transport Container Responsibility: Research Assistant / NINDS EEG Department Staff / MEG Staff. Frequency: After each use Transport to NINDS for cleaning &Cidex disinfection: Research Assistant / NINDS EEG Department Staff / MEG Staff.
- I. Cleaning without Detergents
- A. EasyCap:
- 1. Soak the cap for 30 sec in tap water, while observing proper Infection Control techniques, as soon as possible after use to remove any leftover gel/paste.
- 2. Brush / clean cap with a soft toothbrush, if there is any remaining gel/paste.
- 3. Rinse the cap under running lukewarm tap water.
- 4. Disinfect the cap per manufacturer’s instructions following Hospital Epidemiology Services (HES) / MEG Lab Infection Control policies and procedures.
- A. EasyCap:
- B. Electrodes:
- 1. Brush electrodes with a soft toothbrush, while employing proper Infection Control techniques, as soon as possible after use to remove gel/paste.
- 2. Rinse electrodes under running lukewarm tap water.
- 3. Do not immerse the JIF end of the electrode assembly in water; wipe with a hospital approved cleaner or disinfectant.
- 4. Disinfect electrodes per manufacturer’s recommendations using Metricide, Envirocide or Cidex OPA while following CCs / MEG Lab Infection Control policies and procedures.
- *Every so often after rinsing (Step# 2), soak / swish the electrodes in distilled water.
- B. Electrodes:
- II. Cleaning using Detergents
- Detergent is only necessary if the cap or electrodes have been in contact with a fatty/greasy substance such as sweat, hand cream, styling products, gel, hair oil or dirt. Do not use dish detergents as they leave a film on the surface of cleaned electrodes, which impedes achieving good electrode impedances. Use “pure” soap or shampoo; Castile Soap or baby shampoo provides a better option.
- A. EasyCap:
- 1. Pour the detergent into a container of tap water.
- 2. Soak the cap for 30 to 60 seconds in tap water as soon as possible after use to remove any leftover gel/paste.
- 3. Brush / clean cap with a soft toothbrush, if there is any remaining gel/paste.
- 4. Rinse the cap under running lukewarm tap water.
- 5. Disinfect the cap per manufacturer’s recommendations using Metricide, Envirocide or Cidex OPA while following CCs / MEG Lab Infection Control policies and procedures.
- A. EasyCap:
- B. Electrodes:
- 1. Pour the detergent into a container of tap water.
- 2. Soak the electrodes for 30 to 60 seconds in distilled water.
- 3. Clean electrodes with a soft toothbrush as soon as possible after use to remove any remaining gel/paste.
- 4. Rinse electrodes under running lukewarm distilled water.
- 5. Disinfect electrodes per manufacturer’s recommendations using Metricide, Envirocide or Cidex OPA while following CCs / MEG Lab Infection Control policies and procedures.
- B. Electrodes:
- III. Disinfection using Cidex OPA
- a. The VSM EasyCap and electrodes will be disinfected in the NINDS EEG Department by the EEG staff using Cidex OPA per manufacturer’s specification and in accordance with the proper use of Cidex OPA as specified by the manufacturer and CC Infection Control policies and procedures.
- b. Please Note:
- 1. Do not leave the electrodes in water for a long period of time.
- 2. Do not immerse / soak the electrode connector / ZIF IN WATER; wipe the ZIF connector with a Clinical Center approved disinfectant, such as hydrogen peroxide.
- 3. Do not expose the cap or electrodes to temperatures over 35 degrees Celsius.
- 4. Changes in surface color can be ignored.
- 5. Measure the continuity of electrodes using an Ohm Meter.
- 6. Broken or damaged individual electrodes are NOT repairable or replaceable.
- III. Disinfection using Cidex OPA
- References:
- 1. National Institute of Health, Clinical Center Hospital Epidemiology Service.
- 2. OSHA Infection Control Guidelines.
- 3. CDC Infection Control Guidelines.
- 4. EasyCap Recommendations / Instructions.
- References:
Drug Studies Infection Control Procedures
National Institute of Mental Health
|
Subject: |
Date: 1/11 |
|
Recommended By: |
Distribution: MEG Core Facility, 7NE Nursing Staff, Hospital Epidemiology Service (HES) |
In addition, all nurses assisting with blood draws in the MEG lab must comply with all Clinical Center Infection Control Policies and Procedures.
Procedures:
- 1. All nurses participating in drug studies in the MEG Lab must attend MEG Lab specific Infection Control training.
- 2. Gloves will be used when drawing blood or whenever touching the blood draw syringe or any potentially contaminated items.
- 3. “Contaminated” gloves will be discarded before touching any other items in the MEG lab.
- 4. After gloves are removed, hands must be washed / sanitized before touching any other “clean” items including MEG equipment, telephone and any computer keyboards.
- 5. All surfaces (prep table, cabinets) will be wiped with Dispatch after use.
- 6. All MEG Lab staff will monitor participants for compliance.
- *Anyone who has not received MEG lab Infection Control training should contact the MEG Lab Manager as soon as possible.
- **MEG staff will monitor hand washing in compliance with the CC Hygiene Initiative.
- *Anyone who has not received MEG lab Infection Control training should contact the MEG Lab Manager as soon as possible.
Quality Assurance and System Risk Management
Calibration Procedures
National Institute of Mental Health
|
Subject: |
Date: 11/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: Calibration procedures should be performed for quality assurance and in order to evaluate the performance of the MEG system.
CALIBRATION PROCEDURE: PERFORM WHENEVER: A. Noise / Gain Measurement -there is line frequency noise B. Head Coil Calibration -head localization results / accuracy is in doubt D. Magnetic Phantom Measurement -the performance of the MEG system is in question C. EEG Gain Calibration -EEG results are uncertain
Reference: 1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
MEG Noise Collection
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: Noise collection calibration procedures will be performed for quality assurance whenever necessary to evaluate the performance of the MEG system. Noise collection is performed to determine the noise level of each individual channel. Data is collected with no subject and all noise sources are removed from the immediate vicinity of the MEG system.
I. Procedure for acquiring data:
- 1. Close the door to the MSR. The Magnetic Phantom should not be connected during a noise collection.
- 2. Click” Acq Manager” (or click on the Terminal Screen and type “Acq” at the prompt line; then go to step# 6.)
- a. Click on “Select User”.
- 2. Click” Acq Manager” (or click on the Terminal Screen and type “Acq” at the prompt line; then go to step# 6.)
- 3. Select “meglab”.
- 4. Click on “Launch Acq”.
- 5. Select the study type: “Noise”.
- a. Click on “Ok”.
- 5. Select the study type: “Noise”.
- 6. At the Acq Window:
- a. Click on “Acquire data”.
- 6. At the Acq Window:
- 7. Create Directory? Select “Ok”.
- (If this is the first recording of the day you will need to create a directory)
- 7. Create Directory? Select “Ok”.
- 8. At the Acquisition Monitor Window adjust the scale.
- 9. Click on Start. There are 10 -10 sec trials.
- 10. When the collection is done click “Ok” at the “General Information Window”.
II. Procedure for Plotting the Data:
- 1. At the "General Information Window" click on "Tools".
- 2. Click on DataEditor.
- 3. Click on Set.
- a. Select “MEG Left+ZF ZO” channel array.
- 3. Click on Set.
- 4. Frequency Spectrum Display icon.
- a. Display.
- b. Trial.
- c. Stack all trials.
- 4. Frequency Spectrum Display icon.
- 5. Change y axis to “5f to 10f”. Hit Enter.
- 6. List channels that have increased power on the Daily Log.
- 9. Click on Set.
- a. Select” MEG Right+ZC ZP” channel array.
- 9. Click on Set.
- 10. Frequency Spectrum Display icon.
- a. Display.
- b. Trial.
- c. Stack all trials.
- 10. Frequency Spectrum Display icon.
- 11. List channels that have increased power on log.
Head Coil Calibration
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: Head Coil Calibration will be performed for quality assurance as part of the maintenance and calibration procedures whenever: 1) necessary to evaluate the performance of the head coil, 2) a head coil is replaced or to evaluate the performance of the MEG system.
Two Point Calibration Head Coil Calibration using the Magnetic Phantom
Each coil is placed in two positions on the lower calibration ring of the Magnetic Phantom. Two recordings are collected with the 3 or 4 head coils positioned on the calibration ring to determine the magnetic dipole moments of the head localization coils.
- I. Head Coil Setup:
- 1. Fasten the Head Coils to the calibration points located on the outside surface of the Dewar using the white plastic screws. Plug the other ends into MEG jack box. Head coils are placed as usual with:
- a. The red coil affixed to the right calibration point (if facing the dewar; your left),
- b. The green coil attached to the left side,
- c. The blue in the mid front and
- d. The yellow (spare) mid back.
- 1. Fasten the Head Coils to the calibration points located on the outside surface of the Dewar using the white plastic screws. Plug the other ends into MEG jack box. Head coils are placed as usual with:
- I. Head Coil Setup:
- II. Calibration Program:
- 1. Open a Terminal window.
- a. Type: su meg (lowercase).
- b. Enter password: “omega2000”.
- c. Enter: “calibrateCoils”.
- 1. Open a Terminal window.
- II. Calibration Program:
- III. Calibration Procedures:
- 1. Type “calibrateCoils” at a command line prompt
(or click on the calibrateCoils icon on the desktop). - 2. Verify the head localization parameter file.
- 3. Hit ENTER if correct. (MO15_1609.hz.rp)
- 4. Hit ENTER to backup the current head localization parameter (rp) file and verify serial numbers.
- 5. Do you want to calibrate the ADC? Enter: “YES”.
- 6. DSQ Electronics Setup menu displays.
- 7. Calibrate the ADC units used to apply signals to the head localization coils.
- a. Click on Channel Selector - right arrow. Start @ ADC 15. (calibrate each ADC individually; there are 16 ADC’s)
- b. Click on Start Collection.
- 1. Type “calibrateCoils” at a command line prompt
- III. Calibration Procedures:
- 8. Click on File.
- 9. Exit.
- 10. Do you want to enter coil frequencies manually? Enter Y for yes.
- 11. To accept frequency values for coils hit ENTER.
- IV. Starting Data Collection #1
- 1. Hit ENTER to launch Acq to start Data Collection #1.
- 2. Hit ENTER to select turn reference channels off.
- 3. Once Acq has started click on Acquire Data.
- 4. At the Question Menu click Yes.
- 5. Click OK for the folder name if asked.
- 6. Decrease scale.
- 7. When data starts scrolling across the screen, click on the Start button.
- 8. When the window appears indicating that trial #1 has been collected, click the OK button.
- 9. Select Close Window menu item from the File Menu.
- 10. Select Exit from the File Menu.
- 11. When Acq exits, hit the ENTER <Y> key to verify the data set collected.
- IV. Starting Data Collection #1
- V. Starting Data Collection #2
- 1. Swap the head coils for the second data collection:
- a. Swap the left (green) with the right (red) head coil;
- b. Swap the front (blue) with the back (yellow) head coil.
- 1. Swap the head coils for the second data collection:
- V. Starting Data Collection #2
- 2. Hit ENTER to launch Acq for Data Collection #2.
- a. Hit ENTER to select turn reference channels off.
- b. Once Acq has started click on Acquire Data.
- c. At the Question Menu click “Yes”.
- d. Decrease scale.
- e. When the window appears indicating that trial #2 has been collected, click the OK button.
- f. Select Close Window menu item from the File Menu.
- g. Select Exit from the File Menu.
- h. When Acq exits, hit the ENTER <Y> key to verify the data set collected.
- 2. Hit ENTER to launch Acq for Data Collection #2.
- 3. The distance between configurations #1 and #2 for each coil will be calculated and displayed. Hit ENTER to accept the distance.
Note: The distance should be 51.49 cm for the Omega-275 System.
- 4. The moments will be calculated for each coil and displayed. Hit ENTER to accept these values.
Note: a typical coil moment is 1.7e+11 to 1.8e+11 (fT*cm3)/A. Our range is: 1.6e+11 to 1.8e+11.
- 5. Hit RETURN to launch Acq (writes values into the parameter (rp) file).
- 6. At the Question “Do you want to use these values/”, click “Yes” or hit the Enter key to accept the results.
- 7. At the prompt “Remove calibration results datasets” hit RETURN to remove.
- 8. Perform a phantom dipole test to verify the new calibration moments.
Magnetic Phantom Measurement
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: Magnetic Phantom procedures are performed for quality assurance whenever necessary to evaluate the performance of the MEG system. Magnetic Phantom Dipole Localization is used to confirm the localization accuracy of the system by energizing a coil at a level similar to that of a brain signal and calculating its position relative to a coordinate system determined by the head localization coils.
I. Magnetic Phantom Setup:
- 1. Place the platform board on the MEG chair under the Dewar.
- 2. Position the Magnetic Phantom (the one with the flat white top) on platform. The energizing cable should be right of center and the Blue Head Coil center.
- 3. Connect the 3 head coils (Red –right; Green –left; Blue –center) to the magnetic phantom.
- 4. Plug the energizing cable from the phantom into the MEG jack box spare slot.
- 5. Raise chair so that the phantom is under the helmet.
- 6. Position all the cables so that they hang straight down and do not touch each other.
II. Running the Calibrate Program from the ACQ Computer:
- 1. Type “Acq”.
- 2. Select Study Type “Calibrate”.
- 3. Select Magnetic Phantom.
- 4. Might get an error message here. Select NO.
- 5. Acquire data.
- 6. Click on Localize Head.
- 7. OK to start localization.
- 8. Continue.
- 9. Start.
- 10. Click on Continue.
- 11. Click on OK.
- 12. Tools menu. Data Editor. Select a set of channels. Expand scale. Drag to pick (pick peak with bar). Display map to check (Select Topograph).
- 13. To perform calculation - Select Tools; Magnetic Dipole Fit; Display LaunchApp.
Report if fit error is > 2 - 2.5 mm.
- 14. Magnetic Dipole Fit
- 15. Position should be 0, 0, and 0 .05
- 16. File. Exit.
- 17. File. Close Window.
- 18. Exit Acq.
EEG Gain Calibration
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: EEG Calibration procedures will be performed for quality assurance whenever necessary to evaluate the performance of the MEG / EEG system and / or if
EEG results are in doubt.
Procedure:
- 1.Touch the gold static button before removing the head box and before inserting the shorting plug.
- 2.If applicable, remove the EEG jack box.
- 3.Mount the green EEG Gain Calibration Card (also called the Shorting Plug) on the amplifier.
- 4. Run Acq for EEG calibration.
- a. Select - Calibrate.
- b. Select - EEG.calib
- 4. Run Acq for EEG calibration.
- 5. At the query “Would you like to save the protocol as the default for the study?” enter NO.
- 6. Click on the WINDOWS menu.
- 7. EEG channel (highlight 64 EEG channels).
- 8. Select Null Offset.
- 9. Select Cal gain.
- 10. At Warning click OK.
- 11. Save.
- 12. Exit Acq; NO (do not save rp file).
- 13. Dsqsetup (To write values to the database).
- 14. File.
- 15. Save as: Type (“today’s date”. rack).
- 16. Click OK.
- 17. Select Exit.
- 18. Record Values in the database. Type “. /recordcaib.py –w” (write to database).
The gain corrections are typically 1.0 + 2%.
References: 1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
MEG Lab System Monitors
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: MEG System Monitors evaluate the performance and integrity of the MEG equipment for quality assurance.
- Procedure:
- I. Oxygen Monitor Level Check:
- 1. AirPure Oxygen Monitor
- • located in the MEG Lab on the wall just outside the MSR (Magnetically Shielded Room);
- • measures the percentage of oxygen (O2) in the MEG lab;
- • this may be an indication of the air exchange in the MSR and/or the general integrity of the Dewar and related equipment.
- 1. AirPure Oxygen Monitor
- 2. Check the monitor and record the readings on the QA / Maintenance Log.
- 3. The O2 level should be at about 20.9%.
- • the normal range is 19.5-22%;
- • a reading of 22.0% indicates an oxygen enriched atmosphere which can promote fires (burning);
- • a reading of 19.5 or less indicates an oxygen deficient atmosphere and can lead to a loss of consciousness and/or asphyxiation.
- 3. The O2 level should be at about 20.9%.
- 4. The alarm will sound if this level decreased below a certain set level; if that happens:
- • open the door to the MSR and both doors to the lab;
- • evacuate lab if necessary;
- • notify the staff scientist or lab director immediately.
- 4. The alarm will sound if this level decreased below a certain set level; if that happens:
- II. He Gas Flow Meter Readings:
- 1. The Gilmont Gas Flow Meter
- • located inside the MSR near the back-left wall;
- • monitors the rate of Helium boil off which gives an indication of the general integrity of the MEG Dewar and related equipment.
- 1. The Gilmont Gas Flow Meter
- 2. Check and record the reading on the QA / Maintenance Log.
- 3. The Gas Flow Rate Meter Sensor level fluctuates
- • should generally be about 28.
- 3. The Gas Flow Rate Meter Sensor level fluctuates
- 4. After a fill the flow rate might get as high as 40 (at 40 the alarm will go off), however, the level should go back down to 28 within a
reasonable period of time after the fill.
- 4. After a fill the flow rate might get as high as 40 (at 40 the alarm will go off), however, the level should go back down to 28 within a
- 5. If this reading is elevated notify the staff scientist or lab director.
- III. Liquid Helium Level Check:
- 1. The AMI Model 135 Liquid Helium Level Monitor
- • located on the stand just outside the MSR;
- • measures the amount of helium inside the MEG Dewar;
- • should never be allowed to go below 0 (zero) and
- • should not exceed 39.0.
- 1. The AMI Model 135 Liquid Helium Level Monitor
- 2. Plug in the monitor cable. The plug is located inside the MSR near the back-left wall.
- 3. Check and record the reading on the QA / Maintenance Log.
- 4. If the level is approaching 0 (zero) a liquid Helium Fill should be performed; notify appropriate lab personnel.
- 5. When filled the Liquid Helium Level should not exceed 39.0.
- 6. If an overfill occurs:
- a. Notify the staff scientist and/or lab director;
- b. Keep the door to the MSR open;
- c. Leave the Dewar at 550 for 12 to 24 hours.
- References:
- 1. MEG/EEG Operation and Technical Reference Manuals, CTF Systems Inc. (www.ctf.com).
- References:
MEG Lab Materials Safety
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: In compliance with OSHA and the Hazard Communication Standard, Material Safety & Data Sheets will be kept for all chemicals used in the MEG lab. The MSDS Manual will be accessible to all users and employees when in the MEG lab to ensure that the information regarding the properties, hazards, safe and appropriate uses are available for all to review.
- Procedure:
- 1. MSD Sheets on all substances / chemicals used in the MEG Core Facility will be kept in a binder located in the MEG lab at the console;
- 2. The MSD Sheets will be available to all MEG users, staff and employees.
Liquid Helium Safety Procedures
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: Users of Liquid Helium will be: 1) familiar with the properties and characteristics of the gases used in the MEG Lab and, 2) knowledgeable about the operation of gas cylinders to ensure that those gases are being used, stored and transported according to NIH safety guidelines and safe laboratory practices.
- Procedure:
- 1. All MEG staff and users must familiarize themselves with the properties of Liquid Helium. Refer to the Material Safety and Data Sheet (MSDS) Manual.
- 2. The contents of Liquid Helium Storage Dewars will be identified with decals, stencils, or other markings on the outside of the Dewar.
- a. Color codes alone or tags hung on the outside of the Dewar are not acceptable.
- b. Dewars lacking proper identification must not be accepted from the vendors.
- 2. The contents of Liquid Helium Storage Dewars will be identified with decals, stencils, or other markings on the outside of the Dewar.
- 3. Liquid Helium Storage Dewars are transported by using the handle to pull the Dewar; they must never be pushed. Always keep the Dewar in the upright position.
- 4. Liquid Helium Storage Dewar will be transported with the Relief Isolation Valve open so that pressure does not build up in the storage dewar.
- 5. The cylinder contents must be permanently attached to the outside of the Dewar. This identification shall not be removed, covered or defaced.
- 6. Liquid Helium will not be used in environmental rooms unless there is adequate ventilation and/or an oxygen monitor with an audible alarm is present and permission has been granted by the Safety Officer.
- 7. Liquid Helium will be handled using the appropriate care and protective equipment, i.e., face shield and cryogloves, as necessary because contact can cause severe frostbite.
- 8. The safety warnings located on the Helium Dewar will always be followed.
- 9. Empty cylinders will be marked “EMPTY”.
- Variance Event / Quality Assurance:
- 1. Cylinder Leak.
- Variance Event / Quality Assurance:
- Course of Action Event:
- 1. Cylinder Leak – if this happens
- a. If there are reasons to believe that a cylinder is leaking, test for the leak by painting soapy water over the valves and connections.
This will indicate most gas leaks. - b. Do not attempt to repair leaks caused by loose valve stem packing.
- c. Leaking storage Dewars of liquid helium will be moved to a well-ventilated area. There is no potential harm if helium does not critically
displace the amount of oxygen. - d. The Dewar must be labeled indicating the problem.
- e. The vendor will be called for pickup.
- f. Assistance can be obtained from the Health and Safety Branch or by contacting the Safety Officer.
- a. If there are reasons to believe that a cylinder is leaking, test for the leak by painting soapy water over the valves and connections.
- 1. Cylinder Leak – if this happens
- Course of Action Event:
MEG Dewar Spontaneous Warmup Safety Procedures
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: All MEG users will be familiar with safety procedures required in the occurrence of a spontaneous warmup event.
- Spontaneous MEG Warmup:
- 1. If the vacuum on the inside of the Dewar becomes soft a spontaneous warm up of the liquid Helium will likely occur resulting in:
- a. Leaking of helium;
- b. Helium Level Meter reading will likely increase dramatically causing the Helium Boil-Off Alarm to go off.
- c. Pressure inside the Dewar MIGHT possibly build up causing helium to leak from the ports on the top of the dewar resulting in helium escaping into
the magnetically shielded room (MSR) causing the Oxygen Alarm to go off.
- 1. If the vacuum on the inside of the Dewar becomes soft a spontaneous warm up of the liquid Helium will likely occur resulting in:
- Spontaneous MEG Warmup:
- 2. In the event of a spontaneous warmup:
- a. Open the door and evacuate the MSR.
- b. Open the door to the MEG lab.
- c. Turn off the rack. Discontinue scanning; the system can not be operated in the warm state.
- d. Turn off the Helium Alarm.
- e. Turn off the Oxygen Alarm.
- f. Fill out an Incident Report. Place a “Do Not Operate / Do not Use” sign on the MSR door.
- g. Notify the lab director or staff scientist as soon as possible.
- 2. In the event of a spontaneous warmup:
- 3. Potential adverse occurrences
- a. Suffocation.
- b. Frostbite, severe.
- 3. Potential adverse occurrences
- 4. Helium can cause rapid suffocation if not used in a well-ventilated area. If dizziness or drowsiness or loss of consciousness occurs:
- a. Remove person to fresh air.
- b. If not breathing, give artificial respiration.
- c. Call a Code Blue (111).
- d. If breathing is difficult, qualified personnel may give oxygen.
- 4. Helium can cause rapid suffocation if not used in a well-ventilated area. If dizziness or drowsiness or loss of consciousness occurs:
- 5. In case of severe frost bite obtain medical treatment immediately.
- References:
- 1. Health and Safety Manual – Chapter 4B, General Safety and Laboratory Policies Compressed Gases (http://wwwcc.nih.gov/od/admin_policy/index.html).
- 2. MEG/EEG Operation and Technical Reference Manuals, CTF Systems, Inc. (www.ctf.com).
- 3. MEG Core Facility Material Safety and Data Sheet (MSDS) Manual.
- References:
Compressed Helium Gas Safety
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: Users of Compressed Helium Gas will be: 1) familiar with the properties and characteristics of the gases used in the MEG Lab and, 2) knowledgeable about the
operation of gas cylinders to ensure that those gases are being used, stored and transported according to NIH safety guidelines and safe laboratory practices.
- Procedure:
- 1. All MEG staff and users must familiarize themselves with the properties of Compressed Helium Gas. Refer to the Material Safety and Data Sheets (MSDS).
- 2. The contents of Compressed Helium cylinders must be identified with decals, stencils, or other markings on the cylinders. Color codes alone or tags
hung around the necks of the cylinders are not acceptable. Cylinders lacking proper identification must not be accepted from the vendors.
- 2. The contents of Compressed Helium cylinders must be identified with decals, stencils, or other markings on the cylinders. Color codes alone or tags
- 3. Helium Cylinders will not be accepted from the vendors unless the valve safety covers are in place and properly tightened.
- 4. Compressed Helium cylinders will be secured always so they cannot fall.
- 5. Valve safety covers will be in place until pressure regulators are ready to be attached.
- 6. The cylinder contents are permanently attached to the cylinders. This identification shall not be removed, covered or defaced.
- 7. Cylinders will be moved on chain equipped hand trucks or carts; they are never rolled or dragged.
- 8. Employees will not attempt to repair cylinders or cylinder valves, or to force stuck or frozen cylinder valves.
- 9. The cylinder valve will not be opened or cracked without first attaching the proper pressure regulator.
- Care of Pressure Regulators and Needle Valves:
- 1. The valve fittings of Liquid Helium cylinders must be valves attachments that are safe for use with Liquid Helium. Use of adapters to connect regulators to cylinder
valves defeats this safeguard and is not authorized. Only pressure regulators and needle valves approved for the compressed Liquid Helium gases may be used.
- 2. Threads and points of unions must be clean. These surfaces must be inspected before they are connected.
- 3. When attaching regulators or needle valves, the connections must be tightened firmly. Wrenches of the proper size should be used. Pliers should not be used
as they damage the soft brass nuts.
- 3. When attaching regulators or needle valves, the connections must be tightened firmly. Wrenches of the proper size should be used. Pliers should not be used
- 4. Do not apply excessive force when attaching the regulator or valve. Need for excessive force often indicates that the regulators or needle valves do not fit the cylinders.
- 5. Leaks at the unions between the regulators and the cylinder valves are usually due to damage to the faces of the connections. Attempts to force a tight fit may damage
the previously undamaged half of the connection.
- 5. Leaks at the unions between the regulators and the cylinder valves are usually due to damage to the faces of the connections. Attempts to force a tight fit may damage
- 6. If the cylinder valve faces are damaged, the cylinders will be returned to the vendors. Employees will not attempt to repair them.
- 7. Damaged regulators will not be used until repaired.
- Checking for Cylinder Leaks:
- 1. Unless there are reasons to believe that cylinders are leaking, testing for leaks may be done after the pressure regulators are
attached to the cylinder valves and the valves opened.
- 2. Soapy water painted over the valves and connections will be performed if a leak is suspected.
- 3. Personnel will not attempt to repair leaks caused by loose valve stem packing.
- 4. Leaking cylinder of compressed Helium gas will be returned to the vendor.
- 5. Assistance can be obtained from the Health and Safety Branch or by contacting the Safety Officer.
- Care of Empty Cylinders:
- 1. A small amount of gas must be left in the cylinders and the cylinder valves must be closed to prevent contamination of the inside of the cylinders.
- 2. Empty cylinders should be marked “EMPTY”.
- 3. Valve safety covers and the labels showing contents must be in place.
- 4. Empty cylinders should be stored separately from full cylinders.
- 5. Empty cylinders must be secured at all times so they can not fall.
- Reference:
- 1. Health & Safety Manual – General Safety and Laboratory Policies Compressed Gases (http://www.niehs.nih.gov/odhsb/manual/man4b.htm).
- Reference:
Compressed Helium Gas Level Check (10.40)
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: The Compressed Helium cylinder gas level must be checked by MEG staff once a month in a manner consistent with NIH safety guidelines and safe laboratory practices.
- Procedure:
- 1) All MEG staff will familiarize themselves with the properties of Helium gas. Refer to the Material Safety and Data Sheet (MSDS).
- 2) Close the top valve of the Helium cylinder.
- 3) Turn the knob on the pressure gauge clockwise to open then quickly release. This will vent some helium gas.
- 4) Record the pressure level, as indicated by the pressure gauge, on the Helium Refill Log.
Liquid Helium Refill Procedure
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: The MEG Dewar will be refilled before the Helium level reaches 0 as measured by the AMI Liquid Helium Level Monitor. Liquid Helium refilling procedures will be conducted in a safe manner per manufacturer guidelines.
- Procedure:
- 1. The MEG Dewar liquid Helium level will be checked on a regular basis to determine when to schedule and perform a refill.
- 2. The MEG Dewar will be re-filled before the Helium level reaches 0 as measured by the AMI Liquid Helium Level Monitor (Model 135).
and loses or dissipates about 10% of its volume per day.
- 3. Order Liquid Helium Dewar as needed. Assure that there is a tank / Liquid Helium Dewar on hand with at least 40 liters of helium. It takes about 40 liters for a fill (20 liters to fill the Dewar and about 20 liters to cool the transfer line.
- 4. Assemble all the necessary equipment:
- a. Cryogloves
- b. Dip Stick
- c. LHe Superconducting Dipstick Detector - Model 160
- d. Tape Measure
- e. Clamp
- f. O-Ring
- g. Electric Cord for Heater
- h. Vent Tube and Foam Pad
- i. Storage Dewar
- j. KimWipes
- 4. Assemble all the necessary equipment:
- 5. A Helium Fill procedure will never be left unattended.
- 6. Position the Storage Dewar / Release Pressure.
- a. Move the ceiling tile above the entrance to the Magnetically Shielded Room (MSR) to provide an opening for the Dip Stick.
- 6. Position the Storage Dewar / Release Pressure.
- b. Transport the Helium Storage Dewar to the lab and position in front of the MSR door under the open ceiling tile.
- c. During transport of the LHe Dewar the Relief Isolation Valve (green handle) should be in the open position.
- d. The Primary Relief Valve (blue handle) and the Liquid Withdrawal Valve (yellow handle) should be in the closed position during transport.
- e. After positioning the Dewar at the MSR door, OPEN the Primary Relief Valve (blue handle) to release He gas that has accumulated because
of moving the Dewar.
- e. After positioning the Dewar at the MSR door, OPEN the Primary Relief Valve (blue handle) to release He gas that has accumulated because
- 7. Measure the MEG LHe Sensor Level – This measures the amount of Liquid Helium in the MEG Dewar / Turn Off the Helium Alarm.
- a. Shut off external Helium Flow Meter alarm which is located outside of MSR on the wall adjacent to the rack.
- b. Plug in the cable to the Flow Rate Meter Level Sensor (LHe Level Sensor Cable Monitor) which is located on the back wall inside the MSR.
- c. Turn on the LHe Level Sensor Monitor unit which is located on the stand just outside the MSR. Record the level on the LHe Refill Log.
- d. Raise or lower the MEG Dewar to a 15-degree tilt. Allow time to let the Helium settle before beginning fill procedures.
- 8. Measure the Storage Dewar LHe Level
- a. Wipe the Dip Stick.
- b. Remove the metal plug from the top of the Storage Dewar. Check and adjust the retainer and the O-ring.
- c. Open the Liquid Withdrawal Valve (yellow handle).
- d. Open the Primary Relief Valve (blue handle) is open. *The Isolation Valve (green handle) should already be in the open position.
- e. Slowly insert the Dip Stick in the storage Dewar.
- f. After the Dip Stick reaches the bottom place a clip on the Dip Stick at the point where it meets the top of the Christmas tree.
- g. Connect the LHE Superconducting Dipstick Detector to the Dip Stick.
- h. Set the LHe Superconducting Dipstick Detector to GAS DETECT.
- i. Slowly raise the Dip Stick until it is no longer in liquid and the alarm sounds. Do this several times to be sure of the level then
mark with a second clip.
- i. Slowly raise the Dip Stick until it is no longer in liquid and the alarm sounds. Do this several times to be sure of the level then
- j. Remove the Dip Stick from the storage Dewar. Measure the distance between the two clips (in centimeters; from top to bottom).
- k. Record this measurement on the LHe Refill Log.
- 9. Placing the Front End & Pre-Cooling the Transfer Line
- a. Close the Primary Relief Valve (blue handle) and the Relief Isolation Valve (green handle).
- 9. Placing the Front End & Pre-Cooling the Transfer Line
- b. Hang the back end (bellow end) of the Transfer Line using the nylon ceiling support straps.
- c. Uncoil the Transfer Line and hang the front end (elbow end) using the nylon ceiling support straps.
- d. Wipe both ends of the transfer line.
- e. If necessary, adjust the O-ring located at the top of the Storage Dewar (Christmas tree) so that the transfer line will fill snuggly
in the storage Dewar.
- e. If necessary, adjust the O-ring located at the top of the Storage Dewar (Christmas tree) so that the transfer line will fill snuggly
- f. Slowly insert long elbow end tip of the transfer line into the storage Dewar. This procedure expels O2 from the Dewar and also rids the
transfer line of O2 and any frozen condensation.
- f. Slowly insert long elbow end tip of the transfer line into the storage Dewar. This procedure expels O2 from the Dewar and also rids the
- g. The bellow end (small diameter) of the LHe Transfer Line should be outside the MEG Dewar (free) during this process.
- h. After the “flame” is seen (white gas emissions which resembles a flame) open the Primary Relief Valve (blue handle).
- i. Plug in the (orange) heater cord. *Do not turn on until the bellow end of the transfer line has been inserted and secured.
- j. When the bellows end has been insert in the MEG Dewar and the clamps have been secured CLOSE the Primary Relief Valve (blue handle).
- 10. Placing the Back End of The Transfer Line / Vent Port Tube Placement & Starting the LHe Transfer
- a. Vent Port Tube Placement
- 1. Open the Vent Port carefully; the LHe reservoir is pressurized. *Be careful not to allow your hand or fingers to come in
contact with the cold vapor.
- 1. Open the Vent Port carefully; the LHe reservoir is pressurized. *Be careful not to allow your hand or fingers to come in
- a. Vent Port Tube Placement
- 10. Placing the Back End of The Transfer Line / Vent Port Tube Placement & Starting the LHe Transfer
- 2. Remove the Vent Port Valve and the O-ring.
- 3. Place the O-ring on the Vent Tube then insert the Vent Tube into the Vent Port.
- 4. Place the Foam Padding under the rubber tubing and direct the gas flow away from the gantry.
- 5. Secure with the clamp.
- b. Fill Port / Transfer Line Placement
- 1. Wipe the bellow end of the transfer line.
- b. Fill Port / Transfer Line Placement
- 2. Open the Fill Port. Remove the Fill Port Clamp, Valve and O-ring.
- 3. Place the O-ring on the end of the transfer line and slowly insert the transfer line in the fill port.
- 4. Care should be taken not to bend the transfer line at the joint. Place and tighten the clamp.
- c. Heater - Turn on the heater for just a second or two to increase the pressure. The pressure should be at about 5 Psi.
- d. Once the transfer is under way periodically check the LHe Level Sensor Monitor (located on the stand outside the MSR). F
ill the MEG Dewar to about 36-38 cms (max is 40.8 cm).
- d. Once the transfer is under way periodically check the LHe Level Sensor Monitor (located on the stand outside the MSR). F
- e. After the fill is complete stop the transfer by opening the Primary Relief Valve (blue handle) to depressurize the transfer line.
- 11. Post-Transfer Procedures:
- a. Remove the bellow end of the transfer line from MEG Dewar Fill Port. Replace the Fill Port Valve, O-ring and clamp.
Wear Cryogloves during this procedure.
- a. Remove the bellow end of the transfer line from MEG Dewar Fill Port. Replace the Fill Port Valve, O-ring and clamp.
- 11. Post-Transfer Procedures:
- b. Remove (blow) the frost from the Vent Tubing before opening the Vent Port.
- c. Remove the Vent Tube from the vent port. Replace the frozen Vent Port Clamp and O-ring with others.
- d. Remove the elbow end of the transfer line from the storage Dewar. *Wear Cryogloves during this procedure.
- 12. Measure Post-Transfer Storage Dewar Level:
- a. Measure the LHe level in the storage Dewar with the Dip Stick. Record on the LHe Refill Log.
- 12. Measure Post-Transfer Storage Dewar Level:
- b. Close the Liquid Withdrawal Valve (yellow handle); Close the Primary Relief Valve (blue handle) and open the Relief Isolation Valve (green handle)
for transport. *Refer to the labels on the Dewar.
- b. Close the Liquid Withdrawal Valve (yellow handle); Close the Primary Relief Valve (blue handle) and open the Relief Isolation Valve (green handle)
- c. Unplug the heater and return cord to wall mount.
- 13. Measure Post Transfer MEG Dewar Level:
- a. Measure and record the MEG Dewar LHe level from the LHe Level Sensor Monitor with the Dewar at 15 degrees. Allow the helium to settle for a
bout 10-15 minutes before taking the measurement.
- a. Measure and record the MEG Dewar LHe level from the LHe Level Sensor Monitor with the Dewar at 15 degrees. Allow the helium to settle for a
- 13. Measure Post Transfer MEG Dewar Level:
- b. Unplug the LHe Level Sensor Monitor.
- c. Turn OFF the LHe Level Sensor Monitor unit which is located on the stand just outside the MSR. Record the level on the LHe Refill Log.
- 14. Clean Up:
- a. Return transfer line and vent tube to wall mount; return all other equipment to the proper place.
- 14. Clean Up:
- b. Turn on external Helium flow alarm outside of MSR.
- Adverse Occurrence:
- 1. He Overfill –
- a. Excess He gas from the higher boil off might accumulate in the MSR!
- b. The top plate o-ring might freeze resulting in loss of vacuum (but that would take a long time).
- 1. He Overfill –
- Adverse Occurrence:
- Course of Action for Adverse Occurrence:
- 1. He Overfill
- a. Keep the door to the MSR open so that He gas does not accumulate in the MSR.
- b. Monitor the O2 level in the lab. The O2 level should be at about 20.9% (normal range 19.5-22%).
- c. Don't tilt the system horizontal until the level comes down to below the normal maximum level (about 39 cm). Leave the system overnight with
the Dewar tilt at about 45-degrees from vertical. - d. Monitor the Gilmont 3 flow meter to assure that it comes down to a normal reading (about 27-28 at 150 tilt).
- e. Contact CTF customer support immediately if you notice anything unusual in the cryogenic performance.
- 1. He Overfill
- Course of Action for Adverse Occurrence:
- References:
- 1. Health and Safety Manual – Chapter 4B, General Safety and Laboratory Policies Compressed Gases (www.niehs.nih.gov/odhsb/manual/man4b.htm)
- 2. MEG/EEG Operation and Technical Reference Manuals, CTF Systems, Inc. (www.ctf.com).
- 3. MEG Core Facility Material Safety and Data Sheet (MSDS) Manual.
- References:
Emergency Procedures
Medical Emergency / Possible Seizure Event
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: To define the scope and method for providing immediate action during a possible seizure.
Procedure:
- In the event of a subject has a possible seizure during a MEG study the following steps should be taken.
- I. In the event of a suspected seizure without loss of consciousness:
- 1. If recording, suspend immediately (it is not necessary to stop the acquisition).
- I. In the event of a suspected seizure without loss of consciousness:
- 2. Open the door to the MSR.
- 3. If seated, slide the subject/person out of the chair; If necessary, help the person lie down on the floor. Do not attempt to operate the controls for the chair.
- 4. Assure that the person does not injure himself. Try to remove harmful objects from the person's pathway or coax the person away from those objects.
- 5. Do not try to restrain the person; you cannot stop the seizure. Do not agitate the person.
- 6. If the person appears to be angry or aggressive, do not approach the person if you are alone.
- 7. Observe and document details of the event:
- a. Record the sequence of events.
- b. Note body parts involved.
- c. Record length of event.
- 7. Observe and document details of the event:
- 8. Assess the subject’s level of consciousness.
- 9. Stay with the individual.
- 10. After the event escort victim (or transport via wheelchair) to the Clinical Center office of Occupational Medical Services (OMS) 10/6C306 7:30 am-4:00pm
and / or recommend that the subject seek immediate medical care from their physician.
- 10. After the event escort victim (or transport via wheelchair) to the Clinical Center office of Occupational Medical Services (OMS) 10/6C306 7:30 am-4:00pm
- 11. Ask subject if they have a history of seizures; ask subject if he has any memory of the event. Document information.
- 12. If the subject subsequently loses consciousness and/or the seizure does not terminate after about 5-10 minutes call a Code Blue (111).
- 13. Fill out Problem Report Form (under construction).
- II. In the event of a suspected seizure WITH loss of consciousness:
- 1. If recording, suspend immediately (it is not necessary to stop the acquisition).
- II. In the event of a suspected seizure WITH loss of consciousness:
- 2. Open the door to the MSR.
- 3. Slide the subject out of the chair down to the floor; do not attempt to operate the controls for the chair.
- 4. Assure that the subject does not injure himself.
- a. Put something soft under the head.
- b. Remove any eyeglasses.
- c. Loosen any tight clothes.
- d. Clear the area of sharp or hard objects.
- 4. Assure that the subject does not injure himself.
- 5. DO NOT force anything into the subject’s mouth.
- 6. Do not try to restrain the person; you cannot stop the seizure.
- 7. Observe and document details of the event.
- a. Record the sequence of events.
- b. Note body parts involved.
- c. Record length of event.
- 7. Observe and document details of the event.
- 8. Assess the subject’s level of consciousness.
- 9. Stay with the individual.
- 10. Call 111 to report a Medical Emergency.
- 11. If the subject recovers before emergency personnel arrive, turn the person to one side (rescue position) to allow saliva to drain from the mouth.
- 12. Do not offer the person any fluid or drink.
- 13. Access/monitor for respiratory or cardiac compromise. If necessary, begin rescue breathing or CPR until emergency medical personnel arrives.
- 14. Fill out a Problem Report Form (Under construction).
Medical Emergency / Possible /cardiac or Respiratory Event
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: To define the scope and method for providing immediate action during a medical emergency.
UNRESPONSIVE VICTIM / SUSPECTED CARDIAC OR RESPIRATORY EVENT
Adult Victim: The most common medical emergency in an adult victim is usually a heart attack. The greatest impact on improving the survival from adult sudden cardiac arrest is immediate bystander CPR and defibrillation within 5 minutes. Symptoms of a heart attack might include: pressure / achy pain in the chest, back (between the shoulder blades), jaw, perhaps radiating to the arm, nausea, dizziness, sweating, agitation, indigestion, denial on the part of the subject.
Child/Pediatric Victim: The most common cause of sudden cardiac arrest in infants and children is a lack of oxygen to the heart muscle and brain caused by severe breathing emergencies, respiratory arrest, or shock. The key to survival is early ventilation. Symptoms of a choking victim might include: gasping for air, hand around the neck, cyanosis or pallor and eventually loss of consciousness.
- Procedure:
- 1. If subject is in the MSR, immediately open the door to the MSR. It is not necessary to stop the acquisition.
- Procedure:
- 2. Do not attempt to operate the controls for the chair; simply slide the subject out of the chair down to the floor.
- 3. Check for victim's responsiveness.
- 4. Shout out for "HELP!" / have the other (second) MEG operator/observer go get /call help.
- 5. Call X111 for the emergency medical team. Remember: For an adult victim call first; for a pediatric victim call EMS after 5 cycles (or 2 minutes) of CPR.
- 6. Assess the victim / Initiate CPR:
- a. Open airway;
- 6. Assess the victim / Initiate CPR:
- b. Look, listen, feel for breathing;
- c. Attempt 2 breaths;
- i. If breathes do NOT go in / unable to ventilate there is possibly an obstruction:
- • Reposition the head and attempt ventilation again; if still unable to ventilate;
- • Give 5 abdominal thrusts (if pregnant or obese - chest thrusts);
- • Open then check mouth, sweep to remove seen objects;
- • Attempt to ventilate, if no air goes in, reposition and try again, etc. Continue to try to ventilate along with abdominal thrusts until
successful in dislodging obstruction or victim begins breathing on his own.
- • Attempt to ventilate, if no air goes in, reposition and try again, etc. Continue to try to ventilate along with abdominal thrusts until
- • Check for pulse and respiration after 2 minutes (5 cycles).
- ii. Once breaths goes in, check for:
- • Signs of circulation (or lack thereof) – respiration & heart beat / pulse.
- ii. Once breaths goes in, check for:
- d. If NO pulse (no circulation) and NO respiration, begin chest compressions and continue to ventilate;
- e. If NO pulse (no circulation) but there is respiration, perform chest compressions only,
- f. If pulse is present, but NO respiration continue to ventilate by giving rescue breaths,
- g. If heartbeat and breathing present, turn victim onto the side (in the Rescue or Recovery position to maintain the airway.
Emergency Contacts
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: MEG Users should familiarize themselves with all safety procedures and emergency contacts.
Emergency Numbers Fire / Ambulance - call on campus-111 / off campus-911 Police - call on campus-111 / off campus-911 Chemical / Biological / Radiological - call on campus-111 / off campus-911 Engineering - call 108 Bldg 10 - Employee / Visitor life threatening emergency - call 111 (otherwise report to OMS 10/6C306 496-4411 7:30am – 4:00pm)
NIH Non-Emergency Numbers Fire Department 301 / 496-2372 Police 301 / 496-5685 Occupational Medical Service / Work Related Injuries 301 / 496-4411 Emergency Evacuation Coordinator Building 10/4A13 – Jim Wilson X62862
Reference:
- 1. MEG Core Facility Policy and Procedures Manual.
- 2. MEG Quality Assurance Manual.
- 3. Material Safety and Data Sheets Manual.
- 4. The NIH Clinical Center Emergency Plan, National Institutes of Health (http://intranet.cc.nih.gov/od/emergencyplan/).
- 5. NIH Occupant Evacuation Plan 1430 – (http://www1.od.nih.gov/oma/manualchapters/management/1430/main.html).
- 6. Clinical Center Administrative Policies - http://www.cc.nih.gov/od/admin_policy/index.html .
- 7. Emergency Phone Numbers - http://intranet.cc.nih.gov/od/emergencyplan/attachments/attachments-ii.shtml).
Fire Safety Plan
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: To define the scope and method for immediate, positive and orderly action to safeguard life and property during a fire emergency. The MEG Lab has established a Fire Safety Plan in order to define the scope and method for immediate, positive and orderly action to safeguard life and property during a fire emergency.
- 1. The NIH utilizes a zoned evacuation system. When and if the fire alarm signal sounds and the flashing emergency strobe light has been activated in a particular area the occupants in that zone or area of the building must evacuate the building. This alarm is usually followed by recorded instructions to the occupants. Other areas may not be required to evacuate unless their zone fire alarm system has been activated as well.
- 2 The MEG Core Facility Evacuation Team Leader(s) (ETL) may designate Assistant Team Leaders (ATL) to help with the evacuation.
- 3. During a fire emergency:
- a. The ETL will be responsible for the orderly evacuation of and accounting for all staff, subjects and visitors;
- b. The ATL will help to carry out the instructions of the ETL and assists all patients / visitors in the case of an evacuation.
- 3. During a fire emergency:
- Remember:
R.A.C.E. R - Rescue anyone in danger. A - Activate the nearest fire alarm box and
Dial 911 to notify others in the area of the emergency.C - Confine the fire by closing all doors. E - Evacuate the lab.
- 4. If there is a small fire which may be contained using a fire extinguisher:
- a. The nearest fire extinguisher is located outside the MEG Lab.
- b. Extinguish the fire only if it can be done without endangering anyone, after notifying the NIH Fire Department.
- c. When using a fire extinguisher, fight the fire from a position accessible to an exit to avoid entrapment; if in doubt, evacuate the area and wait for the NIH Fire Department to arrive.
- 4. If there is a small fire which may be contained using a fire extinguisher:
- Remember:
P.A.S.S. A. Pull the safety pin B. Aim the nozzle C. Squeeze the handle and D. Sweep from side to side at the
base of the fire until it goes out.
- 5. Fire Evacuation Procedures:
- a. Close all doors as you leave (close the MSR door if safe to do so).
- b. Walk to the nearest FIRE ALARM PULL STATION which is located in the NMR Center main corridor on the wall between the Waiting Area and the door leading to the main building; activate the alarm.
- c. Dial 111 from the nearest phone.
- d. All staff, subjects, users and visitors must evacuate the zone or the building using the Primary Evacuation Route.
- e. If the Primary Evacuation Route is blocked or inaccessible use the Secondary Route.
- f. The ETL will designate a place away from the building for everyone to meet.
- g. Everyone (all staff, subjects, users and visitors) will report to the ETL and remain
outside at the designated area until all persons have been accounted for or until otherwise instructed by the ETL. - h. Refer to the MEG Emergency Evacuation Floor Plan Map which is posted inside the MEG Lab at each door and also outside the B1/D65B door.
- 5. Fire Evacuation Procedures:
- References:
- 1. The NIH Clinical Center Emergency Handbook, National Institutes of Health.
- 2. NIH Occupant Evacuation Plan 1430 – http://www1.od.nih.gov/oma/manualchapters/management/1430/main.html.
- 3. The Clinical Center Emergency Plan - http://intranet.cc.nih.gov/od/emergencyplan/.
- 4. Clinical Center Administrative Policies - http://www.cc.nih.gov/od/admin_policy/index.html .
- References:
Power Failure
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: To define the scope and method for immediate, positive and orderly action to safeguard life and property during a power failure.
- Procedure:
- 1. MEG Core staff will determine whether to evacuate the lab.
- 2. In the event of a power failure, the emergency backup lights in the lab and the MSR will automatically activate.
- 3. Discontinue testing and evacuate all staff and subjects / patients.
- 4. Turn off all computers and other electrical equipment, if safe to do so.
- 5. Call / contact Maintenance at 496-5862 to report the power outage.
- 6. Notify MEG Core staff.
- 7. If necessary, evacuate to the nearest area which does have power; listen for emergency communications/ announcements over the PA system.
- 8. Return to the facility when power has been restored and / or when it has been determined that it is safe to do so.
- 9. All emergency backup lights and flashlights will be tested once a year to assure that they are operable.
Reference: 1. NIH Occupant Evacuation Plan – 1430, NIH Policy Manual (ttp://www1.od.nih.gov/oma/manualchapters/management/1430/main.html).
Chemical or Biological Materials Incident
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: To define the scope and method for providing immediate action during a chemical or biological materials incident.
- Procedure:
- 1. Leave the room and close doors.
- Procedure:
- 2. Call the Fire Department by dialing 911 (on campus) or 9-911 at leased (off-campus) facilities.
- 3. Remove contaminated clothing and wash any parts of the body which may have come in contact with the hazardous material.
- 4. Do not permit anyone to enter the room/area until the appropriate authorities determine that the area is safe.
- 5. After safely evacuating, any person(s) who may have become contaminated should be restricted to a single staging area and not permitted to move freely to other locations.
Moving to other locations may create a contamination concern to other occupants and/or other areas of the building.
- 5. After safely evacuating, any person(s) who may have become contaminated should be restricted to a single staging area and not permitted to move freely to other locations.
- 6. If a patient or subject is involved, notify the physician in charge and the Chief of Nursing Service or the Nursing Supervisor.
- Reference:
- 1. NIH Occupant Evacuation Plan – 1430, NIH Policy Manual (ttp://www1.od.nih.gov/oma/manualchapters/management/1430/main.html).
- Reference:
Evacuation / Emergency Preparedness Plan
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: To define the scope and method for immediate, positive and orderly evacuation to safeguard life and property during an emergency.
- Procedure:
- 1. One person will be designated the primary Evacuation Team Leader (ETL) for the MEG Core Facility. The evacuation team leader will be responsible for leading the evacuation and accounting for all staff, subjects, and visitors.
- 2. Elevators must NEVER be used for emergency evacuation unless the elevators are under the direction of the fire department, or are equipped with special systems and
are pre-approved for evacuation.
- 2. In the event that an evacuation is ordered, the ETL and/or other MEG Core Facility staff will evacuate the lab including all subjects / visitors.
- 3. All staff and subjects and visitors will report to ETL.
- 4. Individuals with disabilities will be assisted by one or more persons (aides) assigned by the ETL. The aides will assist the individual(s) to the nearest elevator lobby to await evacuation by the fire department.
- 5. Elevators must NEVER be used for emergency evacuation unless the elevators are under the direction of the fire department, or are equipped with special systems and are pre-approved for evacuation.
- 6. Alternate exits should also be used if the primary exit is inaccessible. Refer to the MEG Emergency Evacuation Floor Plan.
- 7. Upon exiting the building, assemble far enough away as not to interfere with the arrival of fire apparatus and the activities of emergency responders, in an area that provides adequate safety for evacuees. Report to the ETL so that everyone is accounted for then wait for further instruction from the ETL.
- 8. Occupants may return to the building only when authorized by the Senior Fire Officer, Police Officer, or the Occupant Emergency Coordinator (OEC).
MEG Lab Emergency Evacuation Team Leaders (ETL)
Building 10 / Floor: B1; Corridor D; Room: 65BPrimary ETL: Dr. Tom Holroyd
Phone: 301 / 402-2362
Bldg/Rm: 10 / B1D65ASecondary ETL: Judy Mitchell
Phone: 301 / 402-2445
Bldg/Rm: 10 / B1D65B
PRIMARY EVACUATION ROUTE – To Loading Dock: *There are 4 or 5 stairs leading down to the sidewalk.
• From the MEG Corridor, turn left down the main NMR Center corridor. • Turn RIGHT at the first corridor (MRI Corridor). • At the end of the MRI Corridor, turn left down the
Animal Corridor; go through the double doors.• Turn right at the exit sign to the loading dock. • Go through the EMERGENCY EXIT double doors to the back loading dock.
SECONDARY EVACUATION ROUTE – West Side Emergency Exit / outside Bld. 10: *There are 6 or 7 stairs leading down to this exit.
• From the MEG corridor, proceed left down the main NMR Center corridor towards room B1D67
(past the signs for the Laboratory of Cardiac Energetics).• Go through the EMERGENCY ONLY EXIT door down the stairs to the outside of the building. • This exit leads to the west side of Building 10.
ALTERNATE EVACUATION ROUTE– Towards Cafeteria/ Elevators / Front of Building 10: • From the MEG corridor, turn right down the main NMR Center corridor towards the nearest exit. • Go through the EXIT door. • Follow the sign to the cafeteria. • This exit leads to the main building towards the cafeteria and elevators,
i.e., toward the front of Building 10
- Reference:
- 1. The NIH Clinical Center Emergency Plan, National Institutes of Health (http://intranet.cc.nih.gov/od/emergencyplan/).
- 2. NIH Occupant Evacuation Plan 1430 – (http://www1.od.nih.gov/oma/manualchapters/management/1430/main.html).
- 3. Clinical Center Administrative Policies - http://www.cc.nih.gov/od/admin_policy/index.html .
- 4. Emergency Phone Numbers - http://intranet.cc.nih.gov/od/emergencyplan/attachments/attachments-ii.shtml).
- Reference:
MEG Lab Traffic Control
National Institute of Mental Health
|
Subject: |
Date: 1/12 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: MEG Lab user traffic and subject / patient arrivals and departures within the MEG Lab will be coordinated and controlled in order to maintain subject / patient confidentiality at all times. MEG lab staff will regulate the orderly and timely flow of subjects, users and other personnel within the lab at all times.
- Procedure:
- 1. When running a MEG scan with a subject, the door(s) to the MEG Lab will be locked at all times. No one, except the user group members and MEG staff, will be allowed to enter the MEG lab until the scan has ended and the subject has exited.
- Procedure:
- 2. If there is a user group with a subject in the lab and they are running over their scheduled time, the next user group cannot bring their subject into the lab until the previous group and their subject has exited the lab.
- 3. If a user group is running a subject and it becomes apparent that they will run over their scheduled appointment time, it is their responsibility to contact the next group to make arrangements with regards to the delay(s) and any other related scheduling issues so that
subject / patient arrival and departure can be coordinated and handled in an orderly manner.
- 3. If a user group is running a subject and it becomes apparent that they will run over their scheduled appointment time, it is their responsibility to contact the next group to make arrangements with regards to the delay(s) and any other related scheduling issues so that
Compliance
Compliance
National Institute of Mental Health
|
Subject: |
Date: 1/03 |
|
Recommended By: |
Distribution: MEG Core Facility |
Policy: MEG Core Facility users and staff will meet all training, education and/or certification standards as required by the NIMH and the NIH.
- Procedure:
- 1. All MEG staff and users will be responsible for following all MEG Lab Policies and Procedures outlined herein.
- 2. MEG staff and users must complete all mandatory trainings as required by the NIH, individual institutes, and the clinical center.
- 3. In addition, these training courses are required by all MEG Core Facility staff who have direct patient / subject contact:
- a. CPR (once every two years)
- b. Universal Precautions/Infection Control (once a year)
- 3. In addition, these training courses are required by all MEG Core Facility staff who have direct patient / subject contact:
- 4. Any users who do not follow all MEG lab policies and procedures may be denied access to the laboratory or asked to complete additional trainings.